Aquatics FAQs
Recommendations for Fully Vaccinated People
COVID-19 Homepage
RRT Composition: COVID-19 Considerations
RRT activation criteria and processes are outlined in the RRT General Guidance, Section 4.1 3. For COVID-19, RRT activation may occur prior to detection of a COVID-19 case in a particular administrative area. Examples include when there is transmission in a neighboring administrative area or when the emergency response system has already been activated (e.g. Emergency Operations Center (EOC) activation or country-equivalent). Given the high risk of COVID-19 person-to-person transmission, countries can consider prepositioning multidisciplinary RRTs prior to large-scale transmission. For more information about this and how RRT activation may fit within the larger emergency response system see the “COVID-19 72-Hour Response Plan Checklist” 8.
RRT Composition
The ability to rapidly deploy is dependent on having trained, ready-to-deploy staff who are capable of filling critically needed roles for the COVID-19 response. In addition to the considerations outlined in the RRT General Guidance, Section 4.2, RRT staffing for COVID-19 can consider the following 3:
- Ensuring health and safety of team members by limiting deployment of those who have certain underlying medical conditions and might be at increased risk for severe illness from COVID-19. 9
- RRT deployment and mobility restrictions due to transmission concerns and/or travel restrictions may require staffing at the subnational levels or in pre-positioned locations
- Wide geographic distribution of COVID-19 cases and response needs may require deploying RRT members to multiple strategic locations throughout the country (e.g. urban centers, transportation hubs, etc.) 10
If an RRT surge roster was not established prior to COVID-19 transmission, consider RRT member emergency recruitment from other ministries, training programs (e.g. Field Epidemiology and Laboratory Training Programs), academia, United Nations agencies, or non-governmental organizations. Focus the roster on only a few key variables such as: contact information, roles, skills, previous response experience, responder training and readiness tracking. These variables can be expanded once outside the RRT Emergency Phase.
RRT ROLES AND SKILLS
An understanding of general RRT roles and skills are outlined in the RRT General Guidance, Section 2.4, and ideally occur in the non-emergency phase; herein we describe some recommended roles and associated skills for a COVID-19 specific RRT 3 . Although the roles on the deploying RRT can vary and should be dictated by the response needs and the specific context the RRT will be responding to as described in the RRT General Guidance, Section 3.2, the following are commonly represented roles for COVID-19 RRTs: Case Management, Epidemiology, IPC, Laboratory, Risk Communication, and Social Mobilization specialists (Figure 2). Example qualifications and responsibilities for the roles can be found in the RRT General Guidance (Appendix 4) 3 .
It is important to acknowledge the distinction between skills and roles. For example, an Infection Prevention and Control (IPC) specialist responding to COVID-19 may be requested to do a variety of activities such as assess use of PPE in healthcare facilities, implement COVID-19 patient triage processes, establish SOPs for personal protective equipment (PPE) use, and/or train healthcare workers (HCWs) on IPC and PPE. Not all IPC specialists will have the skills or relevant experience to conduct all these activities. Therefore, it is important to identify the skills within each role needed for a COVID-19 response so that the most appropriate RRT members can be selected for deployment. Table 1 highlights examples of specific skills relevant to a COVID-19 RRT and role(s) that may fulfill the skills.
Skills
Associated Roles (specialists)
Skills
Interview suspect, probable, and/or laboratory-confirmed COVID-19 cases
Associated Roles (specialists)
Epidemiology, Case Management
Skills
Conduct contact tracing
Associated Roles (specialists)
Epidemiology
Skills
Develop screening questionnaires with up-to-date COVID-19 case definitions
Associated Roles (specialists)
Epidemiology, Case Management
Skills
Analyze and manage COVID-19 data
Associated Roles (specialists)
Epidemiology, Case Management, IPC, Laboratory, Risk Communication, Social Mobilization
Skills
Train HCWs on COVID-19 specimen collection, storage, packaging, and transport
Associated Roles (specialists)
Laboratory, Case Management
Skills
Assess and train HCWs on the use of PPE for COVID19
Associated Roles (specialists)
Case Management, IPC
Skills
Identify HCWs and in-patients with suspect COVID-19
Associated Roles (specialists)
Case Management, IPC, Epidemiology
Skills
Develop and disseminate messaging about COVID-19 symptoms
Associated Roles (specialists)
Risk Communication, Social Mobilization
RRT STRUCTURE
An understanding of general RRT structure and its flexibility during a response can be viewed in the RRT General Guidance, Section 4.2 3. Considering the COVID-19 roles above, the number of RRT members representing each sector and its structure will vary depending on the outbreak characteristics and response needs. For example, although we use the term “team”, COVID-19 RRTs may start with just one epidemiologist or clinician investigating an alert. In an ongoing outbreak, in areas with high case fatality rates (CFRs) there may be an increased need for IPC or Case Management Specialists on the team, but in areas where the CFR is low and the major issue is inadequate contact tracing, it may be more important to increase epidemiology representation on the RRT. Figure 3 provides example RRT structures for possible COVID-19 response scenarios.
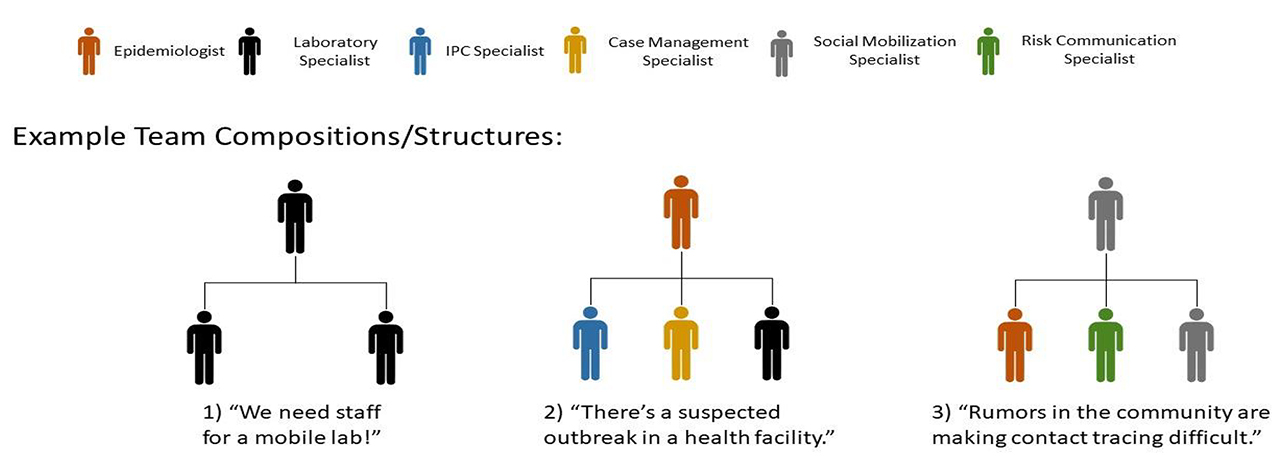
Figure 3: COVID-19 RRT composition/structures using example scenarios
Figure 3 also highlights how the COVID-19 RRTs may have different reporting structures. In the first scenario, the two Laboratory specialists are reporting to a Laboratory specialist Team Lead. In the second scenario, IPC, Case Management, and Laboratory specialists are reporting to an Epidemiologist Team Lead. In the final scenario, there is an Epidemiologist, Risk Communication specialist, and a Social Mobilization specialist reporting to another Social Mobilization specialist Team Lead. These are just illustrative examples of the diversity of expertise that can fill a Team Lead role. Of note, when the deployed RRT is small, the Team Lead can take on dual roles limiting the number of RRT members needed to deploy.
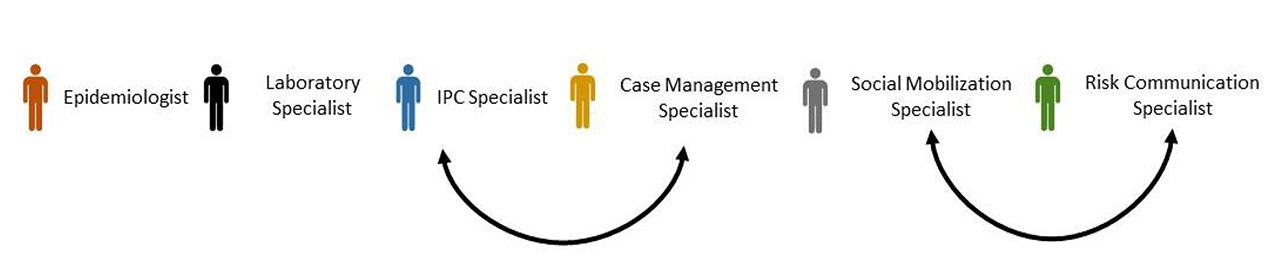
Depending on the need, RRT members can fulfill more than one role on the team. Consider functions with overlapping activities/objectives (e.g., Risk Communication specialist and Social Mobilization specialist, or IPC specialist and Case Management specialist) (see Table 3). When the deployed RRT is small, the Team Lead can take on dual roles limiting the number of RRT members as well.