Aquatics FAQs
Recommendations for Fully Vaccinated People
COVID-19 Homepage
Sharing and Shifting Tasks to Maintain Essential Healthcare During COVID-19 in Low Resource, non-US settings
Purpose
The coronavirus disease 2019 (COVID-19) pandemic has placed a substantial burden on many healthcare systems worldwide as they struggle to treat both COVID-19 patients and maintain essential primary care services. The burden may be even greater in low-resource non-US settings, where healthcare systems are often already overtaxed and struggling to provide services to patients in need due to a shortage in the healthcare workforce.
The World Health Organization (WHO) outlines two approaches to expand and ensure access to essential health services by optimizing the use of the existing healthcare workforce: task shifting and task sharing1 2. Task shifting and task sharing allow for the shifting of tasks from highly qualified healthcare workers (HCWs) to HCWs with less training and less qualifications and the sharing of tasks with an equally qualified cadre of HCWs, respectively. This allows for more efficient use of available human resources working in overburdened health systems during the COVID-19 pandemic.
These two strategies may be one part of a larger strategy to expand and strengthen health system capacity to increase access to COVID-19 care while maintaining essential health services. Additionally, these strategies can help protect and maintain the health and wellbeing of the healthcare workforce by reducing their workload and strategically using staff who are at higher risk of severe illness from COVID-19 in a way that decreases their risk of exposure to the virus that causes COVID-19.
Target Audience
These considerations are intended for countries where access to basic essential health services is constrained due to the COVID-19 pandemic, that have an underlying health workforce shortage, and that are considering implementation of a task shifting or sharing approach to strengthen and expand the health workforce for the delivery of COVID-19 care and other essential health services. Primarily this document is aimed at health care policy makers, program managers and staff in Ministries of Health who manage human resources for health along with local and international organizations providing essential health services that have been affected by the pandemic.
Definitions
Task shifting and task sharing reflect the same intention – to include cadres who do not normally have competencies for specific tasks to deliver them and to thereby increase levels of health care access. Both emphasize the need for training and continued educational support of all cadres of health workers in order for them to undertake the tasks they are to perform. Additionally, routine supportive supervision and a well-functioning referral system are essential preconditions for success. The suggestions in this document generally apply to task sharing and task shifting approaches.
Task shiftingexternal icon is the process of delegation whereby tasks are moved, where appropriate, to less specialized HCWs1. This reorganization of the workforce, along with expanded training and retention programs, can allow a health system to more efficiently use the existing workforce and ease bottlenecks in service delivery while also expanding workforce capacity1 2.
Task sharing increases the categories of HCWs who can deliver certain health services. With task sharing, tasks are not taken away from one cadre or set of HCWs and given to another, but they are shared across groups2. Task sharing enables low- and mid-level health professionals to perform tasks and procedures that would normally be restricted to higher level health professionals, thereby freeing up time for these higher-level providers within a health system.
Basics of Task Sharing and Task Shifting
HCWs may face poor working conditions, low pay, and a sense of being overburdened due to an increase in demand without a comparable increase in a skilled workforce to share the workload in an equitable manner. In addition, in the face of the COVID-19 pandemic frontline HCWs are challenged with putting themselves and their immediate and extended families at risk for contracting the virus that causes COVID-19.
Ultimately the goal of task shifting and sharing in the era of the COVID-19 pandemic is to standardize, simplify, and decentralize systems to maximize the role of primary health care and community based care as it relates to the provision of COVID-19 clinical care1. Good management, supportive supervision, and political will are important for ensuring successful outcomes from task shifting and sharing.
Steps to Consider for Implementation of Task Shifting or Sharing
Given the urgent need to keep essential health services functional during the COVID-19 pandemic, the steps below take into consideration the following: the demand placed on health systems by COVID-19, the legal/ regulatory environment, characteristics of the health system involved, possible resource constraints in low income settings, and what to consider when developing an implementation plan. These steps and considerations have been generalized to be applicable to most situations. Given the uniqueness of each environment in which these steps could be implemented, additional considerations specific to that environment may need to be considered. Additional references and resources can be found in Annex III.
- Determine whether task shifting or sharing is an appropriate intervention
- Assess health system ability to provide COVID-19 services and essential health services.
- Identify appropriate stakeholders to be involved and/or consulted from the beginning
- Develop a nationally endorsed framework for implementation that can ensure harmonization and provide stability for essential primary health care services provided through public and private sectors during the pandemic
- Conduct human resource inventory and assessment to determine demographics and risk of severe COVID-19 symptoms of HCW in public and private sectors
- Assess gaps in essential primary health care service provision and the extent to which task shifting and/or sharing may already be taking place along with existing quality assurance mechanisms
- Assess whether resources are available to support hiring of additional human resources
- Create an enabling regulatory environment for implementation
- Assess existing regulatory approaches (laws, regulations, policies and guidelines) to determine appropriateness of use in implementation
- Undertake revisions as necessary to enable extending scope of practice of different cadres of HCWs and to allow creation of new ones
- Consider adoption of fast-track strategy to produce necessary revisions to regulatory approaches (e.g. some countries may have regulations in place that allow for the establishment of new cadres during periods of national emergency)
- Create an implementation plan that ensures quality of care
- Adapt existing human resource quality assurance mechanisms to support task shifting and/or sharing approaches
- Define roles and competency levels needed for existing HCW cadres and for those that will be newly created under this approach
- Use standards for recruitment, training, and evaluation criteria
- Develop a systematic accredited approach to standardized and competency-based training based on needs
- Ensure all staff are trained on infection prevention and control and appropriate use of personal protective equipment
-
Consider different types of task shifting and sharing practices and adopt/adapt based on local contextSeveral studies that compare non-physician clinicians with medical doctors show minimal differences in outcomes for service users3 and most clinical tasks can be safely and efficiently moved from medical doctors to non-physician clinicians when appropriate training and supervision is provided, and where well-functioning referral systems exist2.
- Determine which providers in outpatient and inpatient settings are underutilized due to cancellations of outpatient visits, non-COVID-19 hospitalizations, and elective procedures, and could be shifted to provide alternate services. See the “Delegation Decision Tree” in Annex I to assist with making these determinations.
- Consider shifting of tasks requiring direct patient care from high risk HCWs to those at lower risk (e.g. based on underlying medical conditions). Annex II has examples of tasks by program area that can be shifted or shared.
- Establish efficient referral systems to support decentralization of service delivery.
- Ensure HCWs are trained on existing referral systems.
- Develop a monitoring and evaluation system
- Provide routine supportive supervision and clinical mentoring using health team model. Performance should be assessed against defined roles and competency levels2
- Develop and implement a standardized and structured evaluation to establish and recognize the ability of HCWs to perform against competency-based standards2
- Successful models include training of supervisors on management, communication, and mentoring skills and recruitment of additional HCWs who will solely assume supervisory tasks2
- Several studies have shown that supportive supervision is conducive to improvements in health worker performance and overall strengthening of health systems2
- Evaluation and outcomes research is important to establish whether tasks that have been shifted or shared result in positive outcomes (i.e. safety and quality of care)
- Establishment of health teams with access to HCWs with higher levels of expertise, skills, and training have been proven to affect performance by HCWs with lower levels of expertise, skills, and training.
Annex I. Sample Delegation Decision-Making Tree
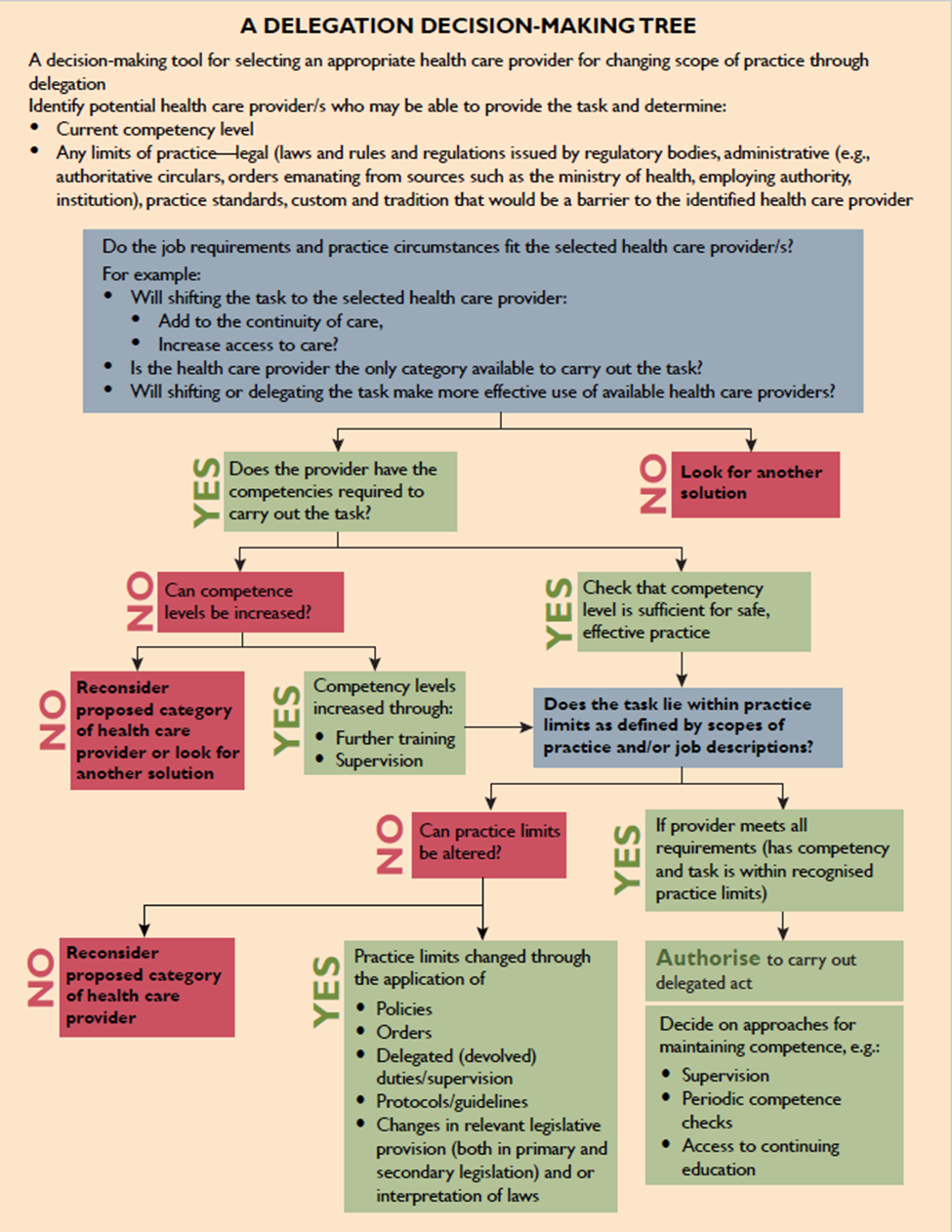
A Delegation Decision-Making Tree
A decision-making tool for selecting an appropriate health care provider for changing scope of practice through delegation
Identify potential health care provider/s who may be able to provide the task and determine:
- Current competency level
- Any limits of practice-legal (laws and rules and regulations issued by regulatory bodies, administrative (e.g., authoritative circulars, orders emanating from sources such as the ministry of health, employing authority, institution), practice standards, custom and tradition that would be a barrier to the identified health care provider
Do the job requirements and practice circumstances fit the selected health care provider/s?
For example:
- Will shifting the task to the selected health care provider:
- Add to the continuity of care,
- Increase access to the care?
- Is the health care provider the only category available to carry out the task?
- Will shifting or delegating the task make more effective use of available health care providers?
Courtesy of JHPIEGO
Annex II
The following table describes examples of tasks under specific health programs that may be shifted or shared. It is assumed that shifting and/or sharing of these tasks comes with adequate training, monitoring, and supervision as described in this document.
Health service: Task shifting and sharing examples
- HIVexternal icon
Community Health Workers (CHW) can:- Distribute refills of antiretroviral therapy (ART) to adults, adolescents, and children living with HIV through home visits, community pick-up points, community adherence groups, etc.1
Non-physician clinicians, midwives, and nurses can:
- Initiate first-line ART or post-exposure prophylaxis, and maintain ART1
- Tuberculosis (TB)
CHWs can:- Screen for TB by identifying people with symptoms (cough greater than 2 weeks, fever, night sweats, and/or weight loss)
Medical doctors, non-physician clinicians, or nurses can:
- Maternal, newborn, and child health service
Antenatal care delivery10:
CHWs, auxiliary nurses, nurses, midwives, and doctors can:- Promote appropriate health-related behaviors
Auxiliary nurses, midwives, and doctors can:
- Distribute recommended nutritional supplements and intermittent preventive treatment in pregnancy (IPTp) to prevent malaria
Skilled care during labor, childbirth and the immediate postnatal period:
CHWs and auxiliary nurses may:- Administer misoprostol to prevent or treat postpartum hemorrhage (PPH) before referral
Auxiliary nurses and auxiliary nurse midwives may:
- Administer intravenous fluid for resuscitation and administer oxytocin as part of PPH treatment
Auxiliary nurse midwives may:
- Deliver neonatal resuscitation
Child health
CHWs can11:
Identify and treat children who have uncomplicated pneumonia, diarrhea or malaria - Non-communicable diseases (NCD) such as hypertension, diabetes, obesity, asthma, and kidney disease
Nurse practitioners, nurses, and CHWs can5:- Provide counseling for patients and family members on medication adherence and address any general concerns12.
- Screen patients with confirmed COVID-19 for a history of preexisting hypertension, diabetes, obesity, asthma, and kidney disease.
- Deliver essential NCD interventions to diagnose, treat and appropriately refer patients with major NCDs
- Use a blood pressure monitoring device, glucometer, pulse oximeter, and nebulizer (NOTE: as nebulizer treatment can generate aerosols, for patients with COVID-19, administration of nebulizer treatments requires appropriate personal protective equipment (PPE): gloves, medical mask (where respirator not available), and eye protection)
- Mental health
CHWs, nurses, psychosocial workers, or community social workers can14:- Raise awareness about mental, neurological and substance use (MNS) care
- Refer people with MNS conditions to seek help at a clinic
- Provide psychological first aid, brief psychological treatments, facilitate self-help groups, teach stress management14.
Annex III. Resources and Relevant Sites
Task Shifting and Task Sharing-general:
-
-
- Global Health Workforce Alliance Resource library on task shiftingexternal icon
- How Surge Staffing Can Fight COVID-19external icon
- Task-shifting: experiences and opinions of health workers in Mozambique and Zambiaexternal icon
- Task Shifting the Management of Non-Communicable Diseases to Nurses in Kibera, Kenya: Does It Work?external icon
-
Surgery and Anesthesia:
-
-
- Task shifting and task sharing for neurosurgeons amidst the COVID-19 pandemicexternal icon
- Bridging the human resource gap in surgical and anesthesia care in low-resource countries: a review of the task sharing literatureexternal icon
- Surgical Task-Sharing to Non-specialist Physicians in Low-Resource Settings Globally: A Systematic Review of the Literatureexternal icon
-
Management of Chronic Conditions:
-
-
- What to Know About HIV and COVID-19
- Task Shifting for Non-Communicable Disease Management in Low and Middle Income Countries-A Systematic Reviewexternal icon
- Task sharing with non-physician health-care workers for management of blood pressure in low-income and middle-income countries: a systematic review and meta-analysisexternal icon
- Task-sharing Interventions for Cardiovascular Risk Reduction and Lipid Outcomes in Low- And Middle-Income Countries: A Systematic Review and Meta-Analysisexternal icon
-
Mental Health:
-
-
- Caring for Children and Adolescents With Eating Disorders in the Current Coronavirus 19 Pandemic: A Singapore Perspectiveexternal icon
- Human resources for mental health care: current situation and strategies for actionexternal icon
- Task Sharing Approaches to Improve Mental Health Care in Rural and Other Low Resource Settings: A Systematic Reviewexternal icon
- Mental Health Collaborative Care and Its Role in Primary Care Settingsexternal icon
-
Maternal, Newborn, and Child Health Care
Economic Impact of Task Shifting:
Considerations in Protecting Healthcare Workers
References
-
-
- WHO, Treat, Train, Retain. The AIDS and health workforce plan. Report on the consultation on AIDS and human resources for health., Geneva: World Health Organization , 2006.
- WHO, Task sharing to improve access to Family Planning/Contraception: Summary brief, Geneva: World Health Organization, 2012, p. 3.
- WHO, Task shifting to tackle health worker shortages, 2007.
- WHO, Task shifting: rational redistribution of tasks among health workforce teams: global recommendations and guidelines, Geneva: World Health Organization, 2008, p. 7.
- WHO, “WHO Recommendations on task shifting components of antenatal care delivery,” 28 March 2018. [Online].
- WHO, Guideline: Managing possible bacterial infection in young infants when referral is not feasible, Geneva: World Health Organization, 2015.
- WHO, Package of essential noncommunicable (PEN) disease interventions for primary health care in low resource settings, Geneva: World Health Organization, 2010.
- WHO, mhGAP Humanitarian Intervention Guide (mhGAP-HIG): clinical management of mental, neurological and substance use conditions in humanitarian emergencies, Geneva: World Health Organization, 2015.
- WHO, Guidelines for treatment of drug-susceptible tuberculosis and patient care, 2017 update, Geneva: World Health Organization, 2017.
- Ariadne Labs, “News: Tackling the Covid-19 Human Resource Emergencyexternal icon,” Ariadnes Labs, June 2020. [Online]. [Accessed June 2020].
- K. Tulenko and N. D’Lima, “MedicineNet: How Surge Staffing Can Fight COVID-19external icon,” MedicineNet, 15 April 2020. [Online]. [Accessed June 2020].
- WHO, Maintaining essential health services: operational guidance for the COVID-19 context: Interim guidance, 1 June 2020, Geneva: World Health Organization, 2020.
- WHO, Operational considerations for case management of COVID-19 in health facility and community: interim guidance,, Geneva: World Health Organization, 2020.
- WHO and UNICEF, Community-based health care, including outreach campaigns, in the context of the COVID-19 pandemic: Interim guidance, May 2020, Geneva: World Health Organization and United Nations Children’s Fund, 2020.
-
