ARCHIVED WEBPAGE: This web page is available for historical purposes. CDC is no longer updating this web page and it may not reflect CDC's current COVID-19 guidance. For the latest information, visit CDC's COVID-19 home page.
Aquatics FAQs
Recommendations for Fully Vaccinated People
COVID-19 Homepage
Interim Operational Considerations for Public Health Management of Healthcare Workers Exposed to or with Suspected or Confirmed COVID-19: non-U.S. Healthcare Settings
The World Health Organization (WHO) provides resources to countries on prevention, identification and management of healthcare personnel infection in the context of COVID-19 pandemic. See WHO guidance: Prevention, identification and management of health worker infection in the context of COVID-19 (who.int)external icon for the most current guidance, resources, and tools.
The U.S. Centers for Disease Control and Prevention (CDC) is working closely with international partners to respond to the coronavirus disease 2019 (COVID-19) pandemic. CDC provides technical assistance to help other countries increase their ability to prevent, detect, and respond to health threats, including COVID-19.
This document is provided by CDC and is intended for use in non-US healthcare settings.
Summary of Recent Changes
1. Background
While new discoveries continue to be made about COVID-19, early reports indicate that person-to-person transmission most often occurs during close contact with an individual infected with SARS-CoV-2, the virus that causes COVID-19. Healthcare workers (HCWs) are not only at higher risk of infection but can also amplify outbreaks within healthcare facilities if they become ill. Identifying and managing HCWs who have been exposed to a patient with COVID-19 is of great importance in preventing healthcare transmission and protecting staff and vulnerable patients in healthcare settings.
2. Target Audience
These operational considerations are intended to be used by healthcare facilities and public health authorities in non-U.S. healthcare settings, particularly focusing on low- and middle-income countries, assisting with the management of HCWs exposed to a person with suspected or confirmed COVID-19.
This includes but is not limited to:
- Healthcare facility leadership
- Infection prevention and control (IPC) staff
- Occupational health and worker safety staff
- Public health staff at the national and sub-national level
3. Objectives
The goals of HCW risk assessment, work restriction, and monitoring are to:
- Allow for early identification of HCWs at high risk of exposure to COVID-19;
- Reinforce the need for HCWs to self-monitor for fever and other symptoms, and avoid work when ill;
- Limit introduction and spread of COVID-19 within healthcare facilities by healthcare personnel;
This document is only intended to advise on the management of HCWs regarding their work within healthcare facilities. Guidance on management of exposed HCWs outside of healthcare facilities (e.g., quarantine, travel-restriction) is beyond the scope of this document. Recommendations are made based on currently available data and subject to change when new information becomes available.
4. Definitions
Healthcare worker – all paid and unpaid persons serving in healthcare settings who have the potential for direct or indirect exposure to patients or their infectious secretions and materials (e.g., doctors, nurses, laboratory workers, facility or maintenance workers, clinical trainees, volunteers).
High risk exposure –
- Close contact for a total of 15 minutes or more with a person with COVID-19 in the community[1]; OR
- Providing direct patient care for a patient with COVID-19 (e.g., physical exam, nursing care, performing aerosol-generating procedures, specimen collection, radiologic testing) without using proper personal protective equipment (PPE)[2] or not performing appropriate hand hygiene after these interactions; OR
- Having contact with the infectious secretions from a patient with COVID-19 or contaminated patient care environment, without using proper personal protective equipment (PPE) or not performing appropriate hand hygiene
Low risk exposure – contact with a person with COVID-19 having not met criteria for high-risk exposure (e.g., brief interactions with COVID-19 patients in the hospital or in the community).
Active monitoring – healthcare facility or public health authority establishes a minimum of daily communication with exposed HCWs to assess for the presence of fever or symptoms consistent with COVID-19[3]. Monitoring could involve in-person temperature and symptom checks or remote contact (e.g., telephone or electronic-based communication).
Self-monitoring – HCWs monitor themselves for fever by taking their temperature twice a day and remaining alert for respiratory and other symptoms that may be compatible with COVID-19. HCWs are provided a plan for whom to contact if they develop fever or even mild symptoms during the self-monitoring period to determine whether medical evaluation and testing is needed.
5. Considerations when Managing HCWs Exposed to Individuals with COVID-19
Healthcare facilities may choose to manage exposed HCWs in a variety of ways and may consider multiple factors when deciding on a management strategy for exposed HCWs, including:
- Epidemiology of COVID-19 in the surrounding community;
- Ability to maintain staffing levels to provide adequate care to all patients in the facility;
- Availability of IPC, employee/occupational health, or other chosen personnel to carry out HCW risk assessment and monitoring activities;
- Access to resources that can limit the burden of HCW active monitoring (e.g., electronic tools)
All healthcare facilities should have an established communication plan for notifying appropriate public health authorities of any HCW who requires testing for COVID-19 during the monitoring period. Staff should be aware of the established procedures for HCWs who have been exposed to a person with COVID-19, and facilities should develop paid sick leave policies and contract extensions that support the ability for staff to avoid work when ill.
Risk Assessment, Work Restriction, and Monitoring
The accompanying flowchart [see Figure] describes possible scenarios for risk assessment of exposed HCWs. Any HCW exposed to a person with COVID-19 in a healthcare facility or in the community should be quickly identified and assessed for fever or symptoms of COVID-19. If found to be symptomatic, they should be immediately restricted from work until a medical evaluation can be completed and testing for COVID-19 considered. If the exposed worker is not symptomatic, an assessment can be done to determine the risk category of exposure, necessary work restriction, and monitoring for 14 days.
Ideally, HCWs who had a high-risk exposure should be restricted from work and remain quarantined with active monitoring for COVID-19 symptoms for 14 days after the date of last exposure. If at any time the worker develops fever or symptoms, they should undergo medical evaluation and COVID-19 testing, if indicated. Those who test negative should continue to be restricted from work, actively monitored, and may return to work at the end of the monitoring period if symptoms are resolved. Those HCWs who remain asymptomatic over the monitoring period may likewise return to work after 14 days. See below Considerations When Resources are Limited for alternative strategies if staffing shortages prevent the ability to restrict HCWs from work.
HCWs who had a low-risk exposure and are considered essential staff may continue to work during the 14 days after their last exposure to a patient with COVID-19. These HCWs should preferably be assigned to care for patients with COVID-19 and should perform self-monitoring twice a day. If the worker is scheduled for a shift, they should take their temperature and self-evaluate for symptoms before reporting to work. Healthcare facilities can consider establishing protocols in which HCWs under self-monitoring report their temperature and symptom status to IPC staff, employee/occupational health, or a designated supervisor prior to beginning a shift. If the HCW develops fever or symptoms, they should:
- Not report to work (or should immediately stop patient care if symptoms begin during a work shift);
- Alert their designated point of contact (POC);
- Be restricted from work until medical evaluation and COVID-19 testing can be performed.
If testing is negative and symptoms are resolved, they may return to work while observing standard precautions and continuing to self-monitor for the remainder of the 14 days. Some facilities have instructed any exposed staff that continue working during the 14 days post-exposure (e.g., asymptomatic low-risk exposure or staff who had symptoms, tested negative and returned to work within the exposure period) to wear a medical mask at all times in the facility to reduce the risk of asymptomatic or pre-symptomatic transmission.
Any HCW who tests positive for COVID-19, either in the course of monitoring after an exposure or otherwise, should be immediately restricted from work and public health notified for further case management.
Considerations When Resources are Limited
There may be situations in which healthcare facilities are unable to perform contact tracing of all HCWs exposed to a patient with confirmed COVID-19 or to carry out an individual risk assessment for all exposed HCWs. Some of these scenarios include:
- Inability to perform contact tracing
Healthcare delivery and traffic flow in a healthcare facility can be dynamic, and documentation of staffing assignments may not be routine practice. This has made it challenging for some healthcare facilities to identify all HCWs who had contact with a case. In situations where identifying all exposed HCWs is not possible, facilities have sent a general communication to all facility staff informing them of:- Exposure risk;
- Associated facility location(s);
- Date(s) and time(s) for potential exposure;
- Instructions for staff to self-identify any known exposures and to notify the designated POC so that risk assessment and public health recommendations can be made;
- Instructions for staff to self-monitor for fever or respiratory symptoms for a chosen period of time and to notify the POC if they become ill.
- Inability to perform individual HCW risk assessments
If many HCWs were exposed to a case or there are limited IPC, employee/occupational health, or public health staff available to assist with public health management, some facilities have found it impractical or impossible to perform individual risk assessments on all exposed HCWs. Efforts have instead focused on identifying staff at highest risk of exposure to COVID-19, including those who were exposed in the setting of an aerosol-generating procedure[4] without the use of appropriate PPE, since this would pose the highest risk of transmission to the HCW. These staff have been designated as potential high-risk exposures, with the remaining exposed staff as potentially exposed. Facilities and public health authorities then determined whether they will manage these staff as low-risk or high-risk while weighing the risks and benefits of each strategy (e.g., available resources, ability to work restrict HCWs, etc.).
- Staff shortages that limit the ability to implement work restrictions
Imposing work restrictions for exposed HCWs may result in staff shortages and potential detriment to patient care for facilities that frequently function over patient capacity or small facilities that maintain only essential staff. In this case, facilities should still perform contact tracing and risk assessment, if possible, with recommended active or self-monitoring depending on the exposure risk level. To avoid critical staffing shortages, some facilities have allowed asymptomatic exposed staff, including those with high-risk exposures, to continue working while wearing a medical mask to reduce the risk of asymptomatic or pre-symptomatic transmission. However, PPE shortages may not allow this strategy to work for many facilities. - Widespread community transmission
In the setting of community transmission, all HCWs are at some risk for exposure to COVID-19, whether in the workplace or in the community. Devoting resources to contact tracing and retrospective risk assessment could divert valuable public health resources away from other important IPC activities. Facilities have instead focused efforts on strengthening routine IPC practices, including:- Reinforce the need for standard precautions for all patient encounters;
- Stress the importance of hand hygiene, cough etiquette, and respiratory hygiene;
- Enforce social distancing between HCWs and patients when not involved in direct patient care;
- Instruct all HCWs at the facility to report recognized exposures;
- Have staff regularly self-monitor for fever and symptoms;
- Remind staff to avoid reporting to work when ill;
- When resources are available, instruct staff to wear a medical mask at all times when in the facility as an additional protective measure to limit potential spread among staff and to patients.
Some facilities have developed a plan for all HCWs to report absence of fever and symptoms to a chosen POC before starting work each day for accountability purposes.
Limited Testing Availability
When overall testing capacity has been limited and must be rationed, facilities and public health authorities have prioritized symptomatic HCWs for testing over low-risk groups in the community (e.g., young healthy individuals). If no testing is available, for the purposes of returning to work, these HCWs have been managed as if potentially infected with SARS-CoV-2 and can return to work based on the strategies described below.
6. Management Considerations of HCWs with Suspected or Confirmed COVID-19
Previous U.S. CDC and WHO recommendations included a symptom-based strategy and a test-based strategy for returning HCWs with suspected or confirmed COVID-19 to work or discontinue isolation. As described in a Decision Memo, U.S. CDC no longer recommends a test-based strategy based on current evidence. This is consistent with a WHO Scientific Briefexternal icon on discontinuation of isolation for COVID-19. Replication-competent virus has not been recovered after 10 days following symptom onset among individuals with mild to moderate COVID-19 illness. In severely or critically ill patients, including some with severely immunocompromising conditions, an estimated 95% no longer have replication-competent virus 15 days after onset of symptoms. While individuals may continue to shed detectable SARS-CoV-2 RNA beyond these time points, a test-based strategy is no longer recommended, with rare exception, because in the majority of cases it results in excluding from work HCWs who continue to shed virus but are no longer infectious.
U.S. CDC recommendations for a symptom-based strategy to determine when HCWs can return to work:
HCWs with mild to moderate illness [5] who are not severely immunocompromised [6]:
- At least 10 days have passed since symptoms first appeared and
- At least 24 hours have passed since last fever without the use of fever-reducing medications and
- Symptoms (e.g., cough, shortness of breath) have improved
Note: HCWs who are not severely immunocompromised and were asymptomatic throughout their infection may return to work when at least 10 days have passed since the date of their first positive viral diagnostic test.
HCW with severe to critical illness5 or who are severely immunocompromised:
- At least 10 days and up to 20 days have passed since symptoms first appeared and
- At least 24 hours have passed since last fever without the use of fever-reducing medications and
- Symptoms (e.g., cough, shortness of breath) have improved
- Consider consultation with infection control experts
Note: HCWs who are severely immunocompromised but who were asymptomatic throughout their infection may return to work when at least 10 days and up to 20 days have passed since the date of their first positive viral diagnostic test.
The exact criteria that determine which HCWs will shed replication-competent virus for longer periods are not known. Disease severity factors and the presence of immunocompromising conditions should be considered in determining the appropriate duration of isolation (see footnotes 5 and 6). Consultation with infection control experts should be considered to determine the optimal time for an individual HCW to return to work.
Per the WHO Scientific Briefexternal icon, countries can choose to continue to use a laboratory testing algorithm as part of the criteria for releasing infected individuals from isolation. Countries that decide to adopt a test-based strategy for returning HCWs to work should take into consideration the limitations of this approach, including HCWs who continue to shed virus but are no longer infectious and strain on testing resources.
CDC and WHO recommend all HCWs wear a medical mask for universal source control if there is SARS-CoV-2 transmission in the community. For countries that are not using medical masks for universal source control, HCWs returning to work after SARS-CoV-2 infection should wear a medical mask at all times while in the healthcare facility until all symptoms are completely resolved or at baseline. After returning to work, HCWs should continue to adhere to hand hygiene, respiratory hygiene, and cough etiquette at all times, and continue to self-monitor for symptoms, seeking medical evaluation if fever or respiratory symptoms worsen or recur.
CDC testing and return to work guidance is based upon currently available evidence and is subject to change as more information becomes available. Please see CDC Criteria for Return to Work for Healthcare Personnel with Suspected or Confirmed COVID-19 (Interim Guidance) for further updates to these recommendations.
Figure: Flowchart for management of HCWs with exposure to a person with COVID-19
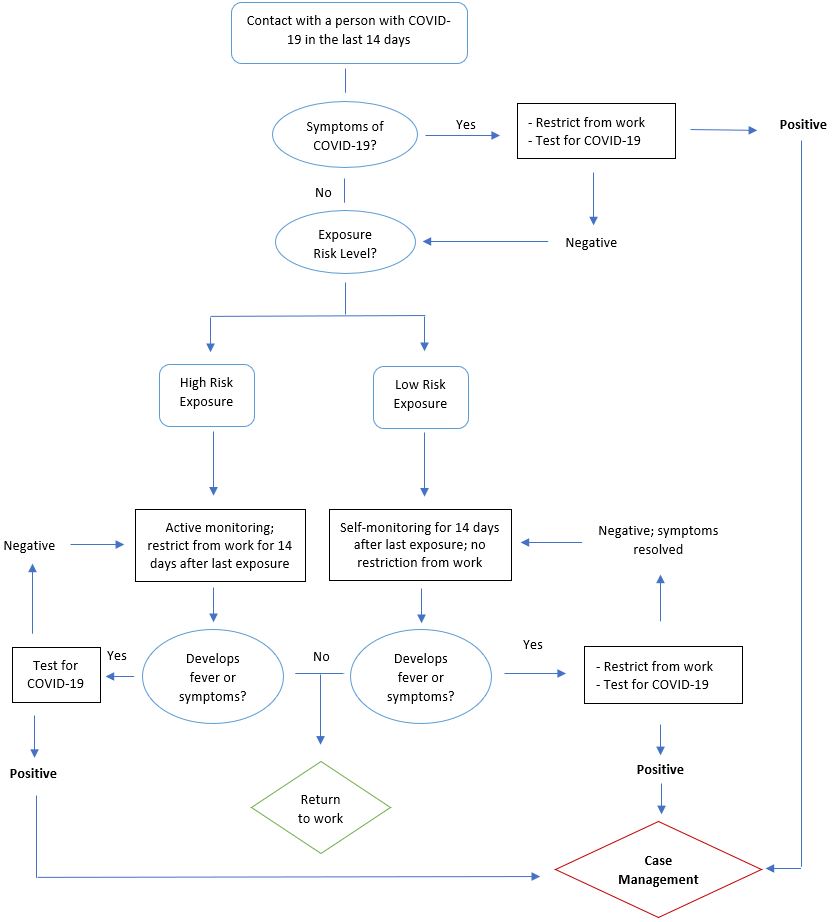
- Contact with a person with COVID-19 in the last 14 days:
- Symptoms of COVID-19?
- If “Yes,” restrict from work and test for COVID-19
- If positive, case management
- If negative, assess exposure risk level
- If “No,” assess exposure risk level
- High Risk Exposure:
- Active monitoring; restrict from work for 14 days after last exposure
- Develops fever or symptoms?
- If “Yes,” test for COVID-19
- If positive, case management
- If negative, return to Active monitoring
- If “No,” return to work
- If “Yes,” test for COVID-19
- Low Risk Exposure:
- Self-monitoring for 14 days after last exposure; no restriction from work
- Develops fever or symptoms?
- If “Yes,” restrict from work and test for COVID-19
- If positive, case management
- If negative and symptoms resolved, return to Self-monitoring for 14 days after last exposure
- If “No,” return to work
- If “Yes,” restrict from work and test for COVID-19
- High Risk Exposure:
7. Additional References
- Centers for Disease Control and Prevention (CDC). Duration of Isolation and Precautions for Adults with COVID-19.
- Centers for Disease Control and Prevention (CDC). Interim U.S. Guidance for Risk Assessment and Public Health Management of Healthcare Personnel with Potential Exposure in a Healthcare Setting to Patients with Coronavirus Disease (COVID-19).
- Centers for Disease Control and Prevention (CDC). Interim US Guidance for Risk Assessment and Public Health Management of Persons with Potential Coronavirus Disease 2019 (COVID-19) Exposures: Geographic Risk and Contacts of Laboratory-confirmed Cases.
- European Centre for Disease Prevention and Control (ECDC). Public health management of persons, including health care workers, having had contact with COVID-19 cases in the European Union – first updateexternal icon.
- Swissnoso. Management of COVID-19 positive or suspect employees involved in care of patients in acute care hospitals.
- World Health Organization (WHO). Advice on the use of masks in the context of COVID-19external icon.
- World Health Organization (WHO). Criteria for releasing COVID-19 patients from isolationexternal icon.
- World Health Organization (WHO). Global Surveillance for COVID-19 disease caused by human infection with the 2019 novel coronavirus – Interim guidanceexternal icon.
- World Health Organization (WHO). Health workers exposure risk assessment and management in the context of COVID-19 virusexternal icon.
Footnotes
1Living in the same household as a person with COVID-19; having direct physical contact with a person with COVID-19 (e.g., shaking hands) or with their infectious secretions (e.g., being coughed on or touching used tissues without gloves); being within 1 meter (CDC guidance recommends to use 6 feet or 1.8 meter) for a total of 15 minutes or more with a person with COVID-19 (e.g., meeting room, workspace, classroom, or traveling in a conveyance); provide direct care to a COVID-19 patient without appropriate PPE per WHO guidance.external icon
2Appropriate PPE as defined by World Health Organization (WHO) Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspectedexternal icon.
3Subjective or measured fever, cough, or shortness of breath. HCW should also monitor for mild or atypical symptoms that have been reported in association with COVID-19, including sore throat, runny nose, fatigue, muscle aches, loss of taste or smell, and gastrointestinal symptoms. For mild or atypical symptoms, medical evaluation and testing should be considered on a case-by-case basis. If index of suspicion is low, can consider continued symptomatic monitoring and reserve testing for new or worsening symptoms.
4Aerosol-generating procedures include, but are not limited to: tracheal intubation, non-invasive ventilation, tracheotomy, cardiopulmonary resuscitation, manual ventilation before intubation, bronchoscopyexternal icon.
5 Adapted from National Institutes of Health COVID-19 Treatment Guidelinesexternal icon.
Mild Illness: Individuals who have any of the various signs and symptoms of COVID-19 (e.g., fever, cough, sore throat, malaise, headache, muscle pain) without shortness of breath, dyspnea, or abnormal chest imaging.
Moderate Illness: Individuals who have evidence of lower respiratory disease by clinical assessment or imaging and a saturation of oxygen (SpO2) ≥94% on room air at sea level.
Severe Illness: Individuals who have respiratory frequency >30 breaths per minute, SpO2 <94% on room air at sea level (or, for patients with chronic hypoxemia, a decrease from baseline of >3%), ratio of arterial partial pressure of oxygen to fraction of inspired oxygen (PaO2/FiO2) <300 mmHg, or lung infiltrates >50%.
Critical Illness: Individuals who have respiratory failure, septic shock, and/or multiple organ dysfunction
6 The studies used to inform this guidance did not clearly define “severely immunocompromised”. For the purposes of this guidance, CDC used the following definition:
- Some conditions, such as being on chemotherapy for cancer, being within one year out from receiving a hematopoietic stem cell or solid organ transplant, untreated HIV infection with CD4 T lymphocyte count < 200, combined primary immunodeficiency disorder, and receipt of prednisone >20mg/day for more than 14 days, may cause a higher degree of immunocompromise and inform decisions regarding the duration of Transmission-Based Precautions.
- Other factors, such as advanced age, diabetes mellitus, or end-stage renal disease, may pose a much lower degree of immunocompromise and not clearly affect decisions about duration of Transmission-Based Precautions.
- Ultimately, the degree of immunocompromise for the patient is determined by the treating provider, and preventive actions are tailored to each individual and situation.