Aquatics FAQs
Recommendations for Fully Vaccinated People
COVID-19 Homepage
Appendices
- Overview
- Scaling Up Staffing Roles
- Training
- When to Initiate
- Investigating a COVID-19 Case
- Contact Tracing for COVID-19
- Source Investigation for COVID-19
- Outbreak Investigations
- Special Considerations
- Building Community Support
- Data Management
- Evaluating Success
- Confidentiality and Consent
- Support Services
- Digital Contact Tracing Tools
- Appendices
Revisions made on January 4, 2022
- Updates made to the public health recommendations listed under the close contact definition.
Revisions made on October 19, 2021
- Based on evolving evidence, CDC recommends fully vaccinated people get tested 5-7 days after close contact with a person with suspected or confirmed COVID-19.
Term
Term
Definition
Definition
Case Investigation & Contact Tracing
Case Investigation & Contact Tracing
Fundamental activities that involve working with a person with COVID-19 (index case) who has been diagnosed with an infectious disease to identify and provide support to people who may have been infected (close contacts) through exposure to the person with COVID-19. This process prevents further transmission of disease by separating people who have (or may have) an infectious disease from people who do not.
Fundamental activities that involve working with a person with COVID-19 (index case) who has been diagnosed with an infectious disease to identify and provide support to people who may have been infected (close contacts) through exposure to the person with COVID-19. This process prevents further transmission of disease by separating people who have (or may have) an infectious disease from people who do not.
Close Contact through proximity and duration of exposure: Someone who was less than 6 feet away from an infected person (laboratory-confirmed or a clinical diagnosis) for a cumulative total of 15 minutes or more over a 24-hour period (for example, three individual 5-minute exposures for a total of 15 minutes). An infected person can spread SARS-CoV-2 starting 2 days before they have any symptoms (or, for asymptomatic people, 2 days before the positive specimen collection date).
- Exception: In the K–12 indoor classroom setting or a structured outdoor setting where mask use can be observed (i.e., holding class outdoors with educator supervision), the close contact definition excludes students who were between 3 to 6 feet of an infected student (laboratory-confirmed or a clinical diagnosis) if both the infected student and the exposed student(s) correctly and consistently wore well-fitting masks the entire time.
This exception does not apply to teachers, staff, or other adults in the indoor classroom setting.
Public Health Recommendations:
People who are identified as close contacts should follow CDC recommendations to protect themselves and others from COVID-19. Recommendations for close contacts to quarantine, get tested, and wear well-fitting masks after exposure to COVID-19 will vary depending on vaccination status and history of prior COVID-19 diagnosis within the past 90 days. People who have come into close contact with someone diagnosed with COVID-19 should follow the recommendations outlined on the COVID-19 Quarantine and Isolation webpage.
Additional Information:
A number of factors can influence a person’s risk of exposure to COVID-19, including the type, proximity, and duration of their exposure, environmental factors (such as crowding and ventilation), vaccination status, COVID-19 infection in the previous 90 days, and mask use.
Correct and consistent mask use is a critical step that people can take to protect themselves and others from COVID-19. In some settings, mask use may be a factor in determining close contact, or in determining recommendations for follow-up after an exposure.
Close Contact through proximity and duration of exposure: Someone who was less than 6 feet away from an infected person (laboratory-confirmed or a clinical diagnosis) for a cumulative total of 15 minutes or more over a 24-hour period (for example, three individual 5-minute exposures for a total of 15 minutes). An infected person can spread SARS-CoV-2 starting 2 days before they have any symptoms (or, for asymptomatic people, 2 days before the positive specimen collection date).
- Exception: In the K–12 indoor classroom setting or a structured outdoor setting where mask use can be observed (i.e., holding class outdoors with educator supervision), the close contact definition excludes students who were between 3 to 6 feet of an infected student (laboratory-confirmed or a clinical diagnosis) if both the infected student and the exposed student(s) correctly and consistently wore well-fitting masks the entire time.
This exception does not apply to teachers, staff, or other adults in the indoor classroom setting.
Public Health Recommendations:
People who are identified as close contacts should follow CDC recommendations to protect themselves and others from COVID-19. Recommendations for close contacts to quarantine, get tested, and wear well-fitting masks after exposure to COVID-19 will vary depending on vaccination status and history of prior COVID-19 diagnosis within the past 90 days. People who have come into close contact with someone diagnosed with COVID-19 should follow the recommendations outlined on the COVID-19 Quarantine and Isolation webpage.
Additional Information:
A number of factors can influence a person’s risk of exposure to COVID-19, including the type, proximity, and duration of their exposure, environmental factors (such as crowding and ventilation), vaccination status, COVID-19 infection in the previous 90 days, and mask use.
Correct and consistent mask use is a critical step that people can take to protect themselves and others from COVID-19. In some settings, mask use may be a factor in determining close contact, or in determining recommendations for follow-up after an exposure.
Confirmed COVID-19 Case
Confirmed COVID-19 Case
Report of person with COVID-19 and meeting confirmatory laboratory evidence.
Report of person with COVID-19 and meeting confirmatory laboratory evidence.
Contact Elicitation Window
Contact Elicitation Window
The timeframe when the case was likely infectious and not under isolation. This is the time period for which possible contacts should be elicited.
The timeframe when the case was likely infectious and not under isolation. This is the time period for which possible contacts should be elicited.
Workers in 16 different sectors pdf icon[810 KB, 19 Pages]external icon including Chemical, external iconCommercial Facilities, external iconCommunications, external iconCritical Manufacturing, external iconDams, external iconDefense Industrial Base, external iconEmergency Services, external iconEnergy, external iconFinancial Services, external iconFood and Agriculture, external iconGovernment Facilities, external iconHealthcare and Public Health, external iconInformation Technology, external iconNuclear Reactors, Materials, and Waste, external iconTransportation Systems, external iconand Water and Wastewater Systems. external iconThese workers include: (a) federal, state and local law enforcement; (b) 911 call center employees; (c) fusion center employees; (d) public and private hazardous material responders; (e) janitorial and custodial staff; (f) workers and contractors in the food and agriculture, critical manufacturing, informational technology, transportation, energy, and government facilities industries. Interim Guidance for Implementing Safety Practices for Critical Infrastructure Workers Who May Have Had Exposure to a Person with Suspected or Confirmed COVID-19 pdf icon[355 KB, 1 Page].
Workers in 16 different sectors pdf icon[810 KB, 19 Pages]external icon including Chemical, external iconCommercial Facilities, external iconCommunications, external iconCritical Manufacturing, external iconDams, external iconDefense Industrial Base, external iconEmergency Services, external iconEnergy, external iconFinancial Services, external iconFood and Agriculture, external iconGovernment Facilities, external iconHealthcare and Public Health, external iconInformation Technology, external iconNuclear Reactors, Materials, and Waste, external iconTransportation Systems, external iconand Water and Wastewater Systems. external iconThese workers include: (a) federal, state and local law enforcement; (b) 911 call center employees; (c) fusion center employees; (d) public and private hazardous material responders; (e) janitorial and custodial staff; (f) workers and contractors in the food and agriculture, critical manufacturing, informational technology, transportation, energy, and government facilities industries. Interim Guidance for Implementing Safety Practices for Critical Infrastructure Workers Who May Have Had Exposure to a Person with Suspected or Confirmed COVID-19 pdf icon[355 KB, 1 Page].
Exposure
Exposure
Having come into contact with a cause of, or possessing a characteristic that is a determinant of, a particular health problem. Principles of Epidemiology in Public Health Practice.
Having come into contact with a cause of, or possessing a characteristic that is a determinant of, a particular health problem. Principles of Epidemiology in Public Health Practice.
First-responder
First-responder
Law enforcement, fire services, emergency medical services, and emergency management officials. EMS Guidance.
Law enforcement, fire services, emergency medical services, and emergency management officials. EMS Guidance.
Healthcare personnel
Healthcare personnel
All paid and unpaid people serving in healthcare settings who have the potential for direct or indirect exposure to people with COVID-19 or infectious materials, including body substances; contaminated medical supplies, devices, and equipment; contaminated environmental surfaces; or contaminated air. Potential Exposure at Work.
All paid and unpaid people serving in healthcare settings who have the potential for direct or indirect exposure to people with COVID-19 or infectious materials, including body substances; contaminated medical supplies, devices, and equipment; contaminated environmental surfaces; or contaminated air. Potential Exposure at Work.
Incubation period
Incubation period
Period of time between exposure to an infection and onset of symptoms
Period of time between exposure to an infection and onset of symptoms
Isolation
Isolation
The separation of a person or group of people known or reasonably believed to be infected with a communicable disease and potentially infectious from those who are not infected to prevent spread of the communicable disease. Isolation for public health purposes may be voluntary or compelled by federal, state, or local public health order.
The separation of a person or group of people known or reasonably believed to be infected with a communicable disease and potentially infectious from those who are not infected to prevent spread of the communicable disease. Isolation for public health purposes may be voluntary or compelled by federal, state, or local public health order.
Multigenerational Household
Multigenerational Household
Households that consist of more than two generations living under the same roofexternal icon. Many researchers also include households with a grandparent and at least one other generation.
Households that consist of more than two generations living under the same roofexternal icon. Many researchers also include households with a grandparent and at least one other generation.
Probable COVID-19 Case
Probable COVID-19 Case
Report of person meeting clinical AND epidemiologic evidence of COVID-19 but without confirmatory laboratory evidence. More about Probable COVID-19 Case pdf icon[252 KB, 10 Pages]external icon.
Report of person meeting clinical AND epidemiologic evidence of COVID-19 but without confirmatory laboratory evidence. More about Probable COVID-19 Case pdf icon[252 KB, 10 Pages]external icon.
Quarantine
Quarantine
The separation of a person or group of people reasonably believed to have been exposed to a communicable disease but not yet symptomatic from others who have not been so exposed to prevent the possible spread of the communicable disease. Quarantine may be voluntary or compelled by federal, state, or local public health order.
The separation of a person or group of people reasonably believed to have been exposed to a communicable disease but not yet symptomatic from others who have not been so exposed to prevent the possible spread of the communicable disease. Quarantine may be voluntary or compelled by federal, state, or local public health order.
When the locating information provided for a person with COVID-19 or close contact is insufficient, case investigation and contact tracing may come to an abrupt halt. The following list includes additional resources that may be used to obtain missing locating information and keep the investigation moving forward.
- State DMV records
- Online people search engines (may incur additional costs)
- Health department records
- Social media/mobile apps
- Following up with the index case to ask for additional locating information on a contact
- Jail and other correctional facility records
- Property tax records
- Frequent shopper cards
- Women Infants and Children Program, Food Stamps and other social services records
- Online white pages
- Google maps
- Employment records
| Data Element | Type | Codes | Notes |
|---|---|---|---|
| Locating Information | |||
| Investigator | Open Text | Name of investigator | |
| Investigator ID | Numeric | ||
| Date Assigned for Investigation | Date | ||
| Index case ID | Numeric | Autogenerated | |
| Lot Number (to link related cases and contacts) | Numeric | To track clusters | |
| Index case Last Name | Open Text | ||
| Index case First Name | Open Text | ||
| Index case Preferred Name | Open Text | ||
| DOB | Date | ||
| Gender | Categorical | M/F/Other/Unk | |
| Primary Language | Open Text/Categorical | ||
| Interpreter used | Categorical | Y/N/U/R | |
| Residential Street Address | Open Text | ||
| City of Residence | Open Text | ||
| County of Residence | Open Text | ||
| State of Residence | Open Text | ||
| Zip code | Numeric | ||
| Tribal Affiliation | Open Text | ||
| Born in the United States | Categorical | Y/N/U/R | |
| Phone Number 1 | Numeric | ||
| Phone Number 2 | Numeric | ||
| Email 1 | Open Text | ||
| Email 2 | Open Text | ||
| Ok to Text | Categorical | Yes, No, Partial, Refused | |
| Ok to Email | Categorical | Yes, No, Partial, Refused | |
| Race | Categorical | Check all apply | Use Census pdf icon[454 KB, 4 Pages]external icon or HHSexternal icon categories |
| Ethnicity | Categorical | Check box | Use Census pdf icon[454 KB, 4 Pages]external icon or HHSexternal icon categories |
| Date of interview Attempt 1 | Date | ||
| Interview 1 occurred | Categorical | Yes, No, Partial, Refused | |
| Date of interview Attempt 2 | Date | ||
| Interview 2 occurred | Categorical | Yes, No, Partial, Refused | |
| Date of interview Attempt 3 | Date | ||
| Interview 3 occurred | Categorical | Yes, No, Partial, Refused | |
| Symptoms and Clinical Course | |||
| Fever | Categorical | Check Box (Y/N/U/R) | |
| Cough | Categorical | Check Box (Y/N/U/R) | |
| Shortness of Breath | Categorical | Check Box (Y/N/U/R) | |
| Diarrhea/GI | Categorical | Check Box (Y/N/U/R) | |
| Headache | Categorical | Check Box (Y/N/U/R) | |
| Muscle ache | Categorical | Check Box (Y/N/U/R) | |
| Chills | Categorical | Check Box (Y/N/U/R) | |
| Sore throat | Categorical | Check Box (Y/N/U/R) | |
| Vomiting | Categorical | Check Box (Y/N/U/R) | |
| Abdominal Pain | Categorical | Check Box (Y/N/U/R) | |
| Nasal congestion | Categorical | Check Box (Y/N/U/R) | |
| Loss of sense of smell | Categorical | Check Box (Y/N/U/R) | |
| Loss of sense of taste | Categorical | Check Box (Y/N/U/R) | |
| Malaise | Categorical | Check Box (Y/N/U/R) | |
| Fatigue | Categorical | Check Box (Y/N/U/R) | |
| Other symptom | Categorical | ||
| Other symptom description | Open Text | ||
| Date of symptom onset | Date | ||
| SARS-CoV-2 testing | Categorical | Check Box (Y/N/U/R) | |
| Date of first SARS-CoV-2 test | Date | ||
| Results of first SARS-CoV-2 test | Categorical | Pos/Neg/Equi/Unk | |
| Date of last SARS-CoV-2 test | Date | ||
| Results of last SARS-CoV-2 test | Categorical | Pos/Neg/Equi/Unk | |
| Hospitalized | Categorical | Yes, No, Partial, Refused | |
| Pneumonia | Categorical | Yes, No, Partial, Refused | |
| ECMO | |||
| ICU | Categorical | Yes, No, Partial, Refused | |
| Death | Categorical | Yes, No, Partial, Refused | |
| Stroke | Categorical | Yes, No, Partial, Refused | |
| MI | Categorical | Yes, No, Partial, Refused | |
| Pre-existing conditions | |||
| Chronic lung disease | Categorical | Yes, No, Partial, Refused | |
| Diabetes | Categorical | Yes, No, Partial, Refused | |
| Severe Obesity (BMI>=40) | Categorical | Yes, No, Partial, Refused | |
| CVD | Categorical | Yes, No, Partial, Refused | |
| Chronic renal disease | Categorical | Yes, No, Partial, Refused | |
| Chronic liver disease | Categorical | Yes, No, Partial, Refused | |
| Immunocompromised | Categorical | Yes, No, Partial, Refused | |
| Pregnant (if Female) | Categorical | Yes, No, Partial, Refused | |
| Risk Factors | |||
| Contact with confirmed COVID case | Categorical | Y/N/U/R | |
| Employed | Categorical | Yes/No-unemployed/No-retired/No-unable to work/No-student | |
| If employed, what occupation | Open text | ||
| If employed, what kind of workplace | Open text | ||
| HCP | Categorical | Y/N/U/R | Work or volunteer in a healthcare setting |
| If HCP, what kind of setting | |||
| Hospital | Categorical | Check box | |
| Ambulatory care | Categorical | Check box | |
| EMS/Fire/Law Enforcement/1st responder | Categorical | Check box | |
| Urgent care | Categorical | Check box | |
| Long term care | Categorical | Check box | |
| Hospice | Categorical | Check box | |
| Name of HCP setting | Open Text | ||
| Address of HCP setting | Open Text | ||
| Congregate setting | Categorical | Y/N/U/R | Do you live or work in congregate setting |
| If Congregate, what kind | |||
| Corrections | Categorical | Check box | |
| Dorm | Categorical | Check box | |
| Group home | Categorical | Check box | |
| Multi-family household | Categorical | Check box | |
| Multi-generational household | Categorical | Check box | |
| Name of congregate setting | Open Text | ||
| Address of congregate setting | Open Text | ||
| Contact Tracing (during contact elicitation window) | |||
| Any household contact | Categorical | Y/N/U/R | |
| Total Number of household contacts | Numeric | ||
| Can you isolate | Categorical | Y/N/U/R | Add in script what this means (use of bedroom and bathroom away from others) |
| Do you need assistance to isolate | Categorical | Y/N/U/R | |
| Any intimate partners | Categorical | Y/N/U/R | Partners you do not reside with |
| Total Number of Intimate Partners | Numeric | ||
| Any other people in close contact with, including coworkers | Categorical | Y/N/U/R |
| Data Element | Type | Codes | Notes |
|---|---|---|---|
| Locating Information | |||
| Investigator | Open Text | Name of investigator | |
| Investigator ID | Numeric | ||
| Date Assigned for Investigation | Date | ||
| Index case’s ID | Numeric | Autogenerated | |
| Lot Number | Numeric | To track clusters | |
| Close contact ID | Numeric | ||
| Contact Last Name | Open Text | ||
| Contact First Name | Open Text | ||
| Contact Preferred Name | Open Text | ||
| DOB | Date | ||
| Gender | Categorical | M/F/Other/Unk | |
| Primary Language | Open Text/Categorical | ||
| Interpreter used | Categorical | Y/N/U/R | |
| Residential Street Address | Open | ||
| City of Residence | Open Text | ||
| County of Residence | Open Text | ||
| State of Residence | Open Text | ||
| Zip code | Numeric | ||
| Tribal Affiliation | Open Text | ||
| Born in the United States | Categorical | Y/N/U/R | |
| Phone Number 1 | Numeric | ||
| Phone Number 2 | Numeric | ||
| Email 1 | Open Text | ||
| Email 2 | Open Text | ||
| Ok to Text | Categorical | Yes, No, Partial, Refused | |
| Ok to Email | Categorical | Yes, No, Partial, Refused | |
| Race | Categorical | Check all apply | Use Census pdf icon[454 KB, 4 Pages]external icon or HHSexternal icon categories |
| Ethnicity | Categorical | Check box | Use Census pdf icon[454 KB, 4 Pages]external icon or HHSexternal icon categories |
| Date of interview Attempt 1 | Date | ||
| Interview 1 occurred | Categorical | Yes, No, Partial, Refused | |
| Date of interview Attempt 2 | Date | ||
| Interview 2 occurred | Categorical | Yes, No, Partial, Refused | |
| Date of interview Attempt 3 | Date | ||
| Interview 3 occurred | Categorical | Yes, No, Partial, Refused | |
| Any household contact | Categorical | Y/N/U/R | |
| Total Number of household contacts | Numeric | ||
| Can you isolate | Categorical | Y/N/U/R | Add in script what this means (use of bedroom and bathroom away from others) |
| Do you need assistance to isolate | Categorical | Y/N/U/R | |
| Symptoms and Clinical Course | |||
| Fever | Categorical | Check Box (Y/N/U/R) | |
| Cough | Categorical | Check Box (Y/N/U/R) | |
| Shortness of Breath | Categorical | Check Box (Y/N/U/R) | |
| Diarrhea/GI | Categorical | Check Box (Y/N/U/R) | |
| Headache | Categorical | Check Box (Y/N/U/R) | |
| Muscle ache | Categorical | Check Box (Y/N/U/R) | |
| Chills | Categorical | Check Box (Y/N/U/R) | |
| Sore throat | Categorical | Check Box (Y/N/U/R) | |
| Vomiting | Categorical | Check Box (Y/N/U/R) | |
| Abdominal Pain | Categorical | Check Box (Y/N/U/R) | |
| Nasal congestion | Categorical | Check Box (Y/N/U/R) | |
| Loss of sense of smell | Categorical | Check Box (Y/N/U/R) | |
| Loss of sense of taste | Categorical | Check Box (Y/N/U/R) | |
| Other symptom | Categorical | ||
| Other symptom description | |||
| Date of symptom onset | Date | ||
| SARS-CoV-2 testing | Categorical | Check Box (Y/N/U/R) | |
| Date of first SARS-CoV-2 test | Date | ||
| Results of first SARS-CoV-2 test | Categorical | Pos/Neg/Equi/Unk | |
| Date of last SARS-CoV-2 test | Date | ||
| Results of last SARS-CoV-2 test | Categorical | Pos/Neg/Equi/Unk | |
| Pre-existing conditions | |||
| Chronic lung disease | Categorical | Yes, No, Partial, Refused | |
| Diabetes | Categorical | Yes, No, Partial, Refused | |
| Severe Obesity (BMI>=40) | Categorical | Yes, No, Partial, Refused | |
| CVD | Categorical | Yes, No, Partial, Refused | |
| Chronic renal disease | Categorical | Yes, No, Partial, Refused | |
| Chronic liver disease | Categorical | Yes, No, Partial, Refused | |
| Immunocompromised | Categorical | Yes, No, Partial, Refused | |
| Pregnant (if Female) | Categorical | Yes, No, Partial, Refused | |
| Risk Factors | |||
| Contact with confirmed COVID case | Categorical | Y/N/U/R | |
| Employed | Categorical | Yes/No-unemployed/No-retired/No-unable to work/No-student | |
| If employed, what occupation | Open text | ||
| If employed, what kind of workplace | Open text | ||
| HCP | Categorical | Y/N/U/R | Work or volunteer in a healthcare setting |
| If HCP, what kind of setting | |||
| Hospital | Categorical | Check box | |
| Ambulatory care | Categorical | Check box | |
| EMS/Fire/Law Enforcement/1st responder | Categorical | Check box | |
| Urgent care | Categorical | Check box | |
| Long term care | Categorical | Check box | |
| Hospice | Categorical | Check box | |
| Name of HCP setting | Open Text | ||
| Address of HCP setting | Open Text | ||
| Congregate setting | Categorical | Y/N/U/R | Do you live or work in congregate setting |
| If Congregate, what kind | |||
| Corrections | Categorical | Check box | |
| Dorm | Categorical | Check box | |
| Group home | Categorical | Check box | |
| Multi-family household | Categorical | Check box | |
| Multi-generational household | Categorical | Check box | |
| Name of congregate setting | Open Text | ||
| Address of congregate setting | Open Text |
Once states have lower COVID-19 case rates for at least 14 days, widely available testing, and adequate medical/hospital resources, contact tracing becomes an important strategy to eliminate transmission of SARS-CoV-2, the virus that causes COVID-19. Contact tracing involves multiple steps, including case investigation of COVID-19 clients, notification of close contacts, and daily monitoring of close contacts. This process can be labor-intensive, and communities have different circumstances that affect contact tracing activities. These factors include the number of persons diagnosed with COVID-19 each day, number of close contacts per index case, and the amount of time and resources needed to reach and follow the clients and contacts. The number of contact tracers needed is large and will vary by community. Each community will need to examine local case load and other factors to estimate how many contact tracers will be needed.
Mathematical modeling tools can be used to help estimate the number of contact tracers needed. These models require data to quantify each part of the process. The data used may differ among communities and over the course of the pandemic, which may lead to large differences in estimates from different models – or from the same model if using different values. Each community will need to determine some key parameters to be in the model. Local tuberculosis / sexually transmitted disease contact tracers are likely familiar with community-specific “inputs” regarding the average number of contacts per case and how difficult contacts are to find.
CDC does not endorse the use of a specific model; however, these tools may be used to guide planning and calculate resources needed under different scenarios. Each community should carefully incorporate as much knowledge about its situation as possible to estimate the number of contact tracers needed.
Content describing non-CDC tools in this document is provided for informational purposes only and is not intended to indicate endorsement, actual or implied, of the tools. Additionally, information on this site is provided “as is,” for users to evaluate and make their own determination as to their effectiveness.
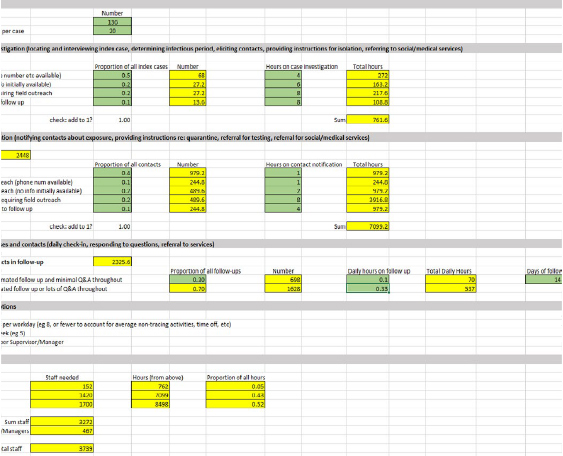
Example using an available tool: Contact Tracing Staffing Tool – Resolve to Save Livesexternal icon
This model is built into an Excel workbook and requires input on the following values:
- # new COVID-19 clients / day
- # close contacts / COVID-19 case
- Proportion of people who are easy / hard / hardest to reach (and never reached). The amount of time needed to arrange and conduct the initial interview with the index person with COVID-19 can vary.
- Average time needed for case investigation for each patient category
- Proportion of contacts who are household / easy / hard / hardest to reach (and never reached). Some close contacts might live with the person with COVID-19; other contacts might lack contact information and require fieldwork to identify.
- Average time spent on contact notification for each contact category
- Proportion of people who can be followed in a mostly automated way versus those who need more staff time. For instance, contacts self-reporting their symptoms via email or text messages require much less time than contacts requiring daily telephone calls.
- Average amount of time spent on contacts for each day in each category
- Days spent following contacts (for example, 14 days after exposure)
- Staffing considerations:
- Hours of daily productive work per contact tracer
- Number of workdays per week per contact tracer
- Number of contact tracers per manager
Changing the parameters in the model will change the estimated total staffing needed, even when keeping the number of daily new COVID-19 cases constant. (Note that this model does not specify overall population size. The total amount of work is proportional to the number of COVID-19 clients and contacts identified in each community rather than the total number of people living in the community.)
| Model developed by Resolve to Save Lives | Assumed daily COVID-19 Incidence/ 100,000 persons | Contact tracing staff needed / 100,000 persons | Notes or assumptions |
|---|---|---|---|
| Contact Tracing Staffing Calculator -Lower estimate (See below) | 9* | 33 | 5 contacts per case; contact tracers work 8 hours/day; contacts easy-to-reach; many contacts use app/email to report daily. |
| Contact Tracing Staffing Calculator – Higher estimate (See below) | 136** | 3,739 | 20 contacts per case; contact tracers work 7-hour days; contacts harder to reach, take longer to interview, most require calls each day. |
*Between April 15-23, 2020, the daily incidence of COVID-19 in the United States ranged between approximately 8 and 9 per 100,000 (between 25,858 and 29,916 new COVID-19 cases per day; assume US population of 328M).
**Approximate peak daily incidence of COVID-19 in New York City (approx. 11,400 incident new cases on 4/15/2020, assume NYC population of 8.4M).
Additional Considerations for Estimating Contact Tracing Resources
There are numerous factors that could affect contact tracer staffing needs that should be accounted for when estimating contact tracer needs:
- These estimates do not necessarily include all managers or additional professions needed.
- Increased case finding and testing efforts, as well as relaxing mobility restrictions could lead to more daily reported COVID-19 cases and/or close contacts, which would require tracing resources.
- Effective contact tracing could reduce the number of new people with COVID-19 and contacts over time.
- Time from diagnosis to isolation for the index patient with COVID-19 will affect the number of people exposed to COVID-19 and needing follow-up.
- Use of digital contact tracing tools pdf icon[391 KB, 2 Pages] could improve workflow efficiency or allow automated messages/contact self-report of symptoms to save contact tracer effort.
- These models do not necessarily apply to special populations such as people in prisons or long-term care facilities.
This information will be updated as more tools become available.
Parameter values used for high and low estimates
(these are for illustrative purposes only)
Low Estimate Values—daily incident cases based on approximate average national daily incidence
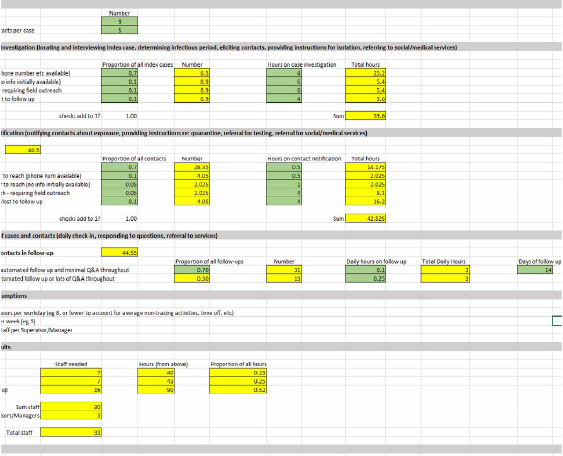
High Estimate Values—daily incident cases based on peak daily incidence from NYC (approx. 11,400 cases among 8.4M persons)