Aquatics FAQs
Recommendations for Fully Vaccinated People
COVID-19 Homepage
Investigating a COVID-19 Case
- Overview
- Scaling Up Staffing Roles
- Training
- When to Initiate
- Investigating a COVID-19 Case
- Contact Tracing for COVID-19
- Source Investigation for COVID-19
- Outbreak Investigations
- Special Considerations
- Building Community Support
- Data Management
- Evaluating Success
- Confidentiality and Consent
- Support Services
- Digital Contact Tracing Tools
- Appendices
Revisions made on November 22, 2020
- Added case investigation and contact tracing prioritization recommendations.
Getting comprehensive information from a patient diagnosed with COVID-19 is the foundation of case investigation and contact tracing. This information includes:
- the case patient’s socio-demographic characteristics,
- history of SARS-CoV-2 (the virus that causes COVID-19) testing and results,
- date of symptom onset, if applicable,
- date of specimen collection for COVID-19 testing,
- source of illness,
- list of close contacts and their locating information,
- duration of exposure,
- the case patient’s activity history during the contact elicitation window (when the patient was infectious and not under isolation),
- exposure locations (including events and gatherings with unknown contacts).
Health departments are responsible for conducting COVID-19 case investigations and contact tracing and often have legal mandates to investigate cases of communicable disease and a duty to notify contacts that they were exposed. Health departments should initiate investigations as quickly as possible. Having written policies and procedures for investigations, including interview guides and call scripts, improves the efficiency and uniformity of investigations. In certain circumstances, it may take more than one interview with a patient to obtain all necessary and accurate information to complete the investigation.
Establishing trust and rapport between a case investigator and a patient diagnosed with COVID-19 is necessary to obtain information and ensure cooperation throughout the investigation. Good interview skills can be taught and will improve with practice. Public health personnel assigned to investigate patients with COVID-19 should be trained in interviewing methods and mentored by experienced employees. Case investigation and contact tracing training guidance and resources are available, including suggestions for role-playing exercises for trainees.
A patient will ideally be interviewed by a case investigator who is fluent in their primary language. If this is not possible, health departments should provide interpretation services, ideally by an individual with an understanding of the patient’s cultural background.
When possible and appropriate, case interviews and contact elicitation should be conducted via telephone call or another distance-based application to ensure the safety of the case investigator and efficient use of program resources.
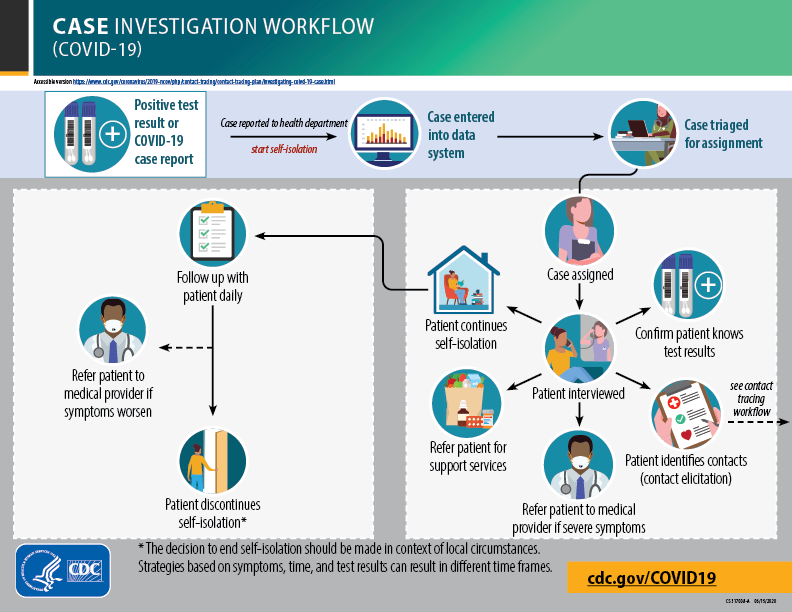
COVID-19 Case Investigation Workflow
Step 1: Case identification & prioritization
COVID-19 case investigations are typically initiated when a health department receives a positive SARS-CoV-2 test result report from a laboratory or a patient’s confirmed or probable diagnosis of COVID-19 from a healthcare provider.
Ideally, jurisdictions will have ample testing available and the public health infrastructure to allow laboratory confirmation of all COVID-19 cases within the community and the capacity to investigate all symptomatic and asymptomatic patients with a confirmed diagnosis of COVID-19.
For guidance on the appropriate use of testing, see Overview of Testing for SARS-COVID-19.
For areas that have limited laboratory testing capacity, prioritization of testing resources should take into consideration the following factors: (1) ensuring optimal care for hospitalized patients and reducing the risk of healthcare-associated infections, (2) ensuring those at higher risk for severe disease are rapidly identified and triaged, and (3) identifying individuals in communities experiencing high numbers of COVID-19 hospitalizations to decrease community spread and ensure the health of critical infrastructure workers.
CDC provides recommended priorities for COVID-19 testing that can be adapted by health departments to respond to rapidly changing local circumstances. CDC’s testing recommendations reinforce the role of case investigation and contact tracing as an effective strategy to decrease community transmission.
Once a COVID-19 laboratory or provider report is received, this information will be entered into the health department surveillance system. With expanded laboratory testing in both public and private sectors, it is important to establish electronic laboratory reporting systems to enhance the timeliness of data to inform public health action.
The health department should use a triage system to use any information known about a patient diagnosed with COVID-19, prior to case interview, to delegate the investigation to either a case investigator or special infection control team (specific settings where a special team is needed are included in Outbreak Investigations).
Health departments can communicate with healthcare providers by phone when a positive laboratory test is reported to obtain information necessary for triaging. Conversely, health departments could request that providers phone-in case information on the same day that a provider receives a positive SARS-CoV-2 test result in a Priority 1 or Priority 2 patient (see Box 1).
In addition to identifying potential outbreaks, information to assist in case prioritization includes a patient’s COVID-19 symptoms, underlying health conditions, locating information (residence type/location/contact information), workplace role and location, confirmation that patient was notified of test result, and initiation of self-isolation.
Triage staff should have rapid turn-around times with provider queries (within 24 hours). Triage staff should then prioritize cases for investigation to either a case investigator or special infection control team based on known information. These strategies are only feasible with adequate staff to provide triage support and sufficient patient information available to allow for prioritizing.
For areas that have limited public health resources to investigate all cases, the case investigation hierarchy (Box 1) and case investigation and contact tracing prioritization recommendations can be used to help guide prioritization when information is known about the case. The hierarchy is based on the assumption that clients with a confirmed or probable diagnosis of COVID-19 in Priority 1 are likely to have exposed a larger number of people and/or are likely to have close contacts who could potentially expose many people, those at higher risk for severe disease, or critical infrastructure workersexternal icon. Priority 2 includes clients who may be at higher risk for severe disease and will need prompt risk assessment and linkage to any needed medical and support services. Clients should be prioritized based on the highest priority category they fall into.
When prioritizing clients with a positive SARS-CoV-2 test result or a probable diagnosis of COVID-19 to investigate, jurisdictions should be guided by the local characteristics of disease transmission, demographics, and public health and healthcare system capacity. Decisions should be supported by local guidance and circumstances.
Box 1. COVID -19 case investigation hierarchy
The case investigation and contact tracing prioritization recommendations are intended to provide additional information and an overview of prioritization strategies for consideration. Implementation should be guided by what is feasible, practical, and acceptable, as well as tailored to the needs of each community.
All confirmed and probable COVID-19 cases should be investigated. When resources are limited, priorities for who should be investigated are listed below. Priority 1 clients are likely to have exposed a larger number of people and/or are likely to have close contacts who could potentially expose: many people, those at higher risk for severe disease, or critical infrastructure workers. Priority 2 clients may be at higher risk for severe disease and will need prompt risk assessment and linkage to any needed medical and support services.
INVESTIGATE CLIENTS WITH A CONFIRMED OR PROBABLE DIAGNOSIS WHO ARE:
PRIORITY 1
- Hospitalized patients
- Healthcare personnel (HCP)
- First responders (e.g., Emergency Medical Services [EMS] personnel, law enforcement, firefighters)
- Individuals living, working or visiting acute care, skilled nursing, mental health, and long-term care facilities
- Individuals living, working or visiting community congregate settings (e.g., correctional facilities, homeless shelters, educational institutions, mass gatherings, and crowded workplaces including production plants)
- Members of a large household living in close quarters
- Individuals known to live in households with an individual at higher risk for severe illness or to provide care in a household with an individual with higher risk for severe illness
- Critical infrastructure workers who work closely with other critical infrastructure workers or are in close contact with large numbers of people (e.g., transportation, food service)
PRIORITY 2
- Critical infrastructure workers who do not work closely with other critical infrastructure workers or are in close contact with large numbers of people (e.g., transportation, food service)
- Individuals 65 years of age and older
- Individuals of any age with certain underlying medical conditions who are at increased risk for severe illness. Pregnant people
PRIORITY 3
- Individuals with symptoms who do not meet any of the above categories
- Individuals who are deceased
PRIORITY 4
- Individuals without symptoms who do not meet any of the above categories
Operational questions to consider
- How are reports received and how are they entered into the database? How complete are the reports?
- Can electronic laboratory reporting for COVID-19 cases be easily implemented?
- How will the time between a client’s symptom onset and self-isolation be assessed? How can delays in laboratory or case reporting, assignment to case investigator, time to client interview and subsequent isolation be monitored?
- How will non-laboratory-confirmed cases be reported by providers and managed by the health department? Will this require a modification of provider reporting requirements and confidential morbidity report forms?
- How will public health staff coordinate with healthcare providers to facilitate testing of probable cases?
- Can laboratory and provider reporting requirements be altered to alert local and state health departments of critical data elements to aid in prioritization?
- Can jurisdictions develop public health alerts to request that providers report probable cases and cases in Priority 1 clients (Box 1) within 24 hours?
- What type of collaborative agreements can be set in place for data sharing between public health and healthcare providers (e.g., access to electronic health records)? How will privacy and confidentiality be maintained?
- For areas with blended state, regional and/or local health department authorities, which entity will be responsible for case prioritization?
- How will investigations be handled for a patient who regularly travels between jurisdictions?
Step 2: Rapid notification of results or diagnosis
- Some clients will have been notified of their positive SARS-CoV-2 test result or probable case diagnosis by their healthcare provider and already received instructions for self-isolation.
- When communication with the client about their positive SARS-CoV-2 test result or probable diagnosis is unclear or has not taken place, the health department should notify the client as soon as possible (within 24 hours of reporting to the health department).
- A client with a probable COVID-19 diagnosis should self-isolate and be linked to testing (if recommended by healthcare providers or state or local public health authorities).
- If there is a need for testing and the case investigator plans to collect the specimen in person, case investigators need to have had appropriate training on infection prevention and control practices. They must also obtain any necessary personal protective equipment (PPE) prior to conducting in-person activities.
- The first connection can be made through different channels such as phone, text, email or in-person (if appropriate) in the primary language of the individual. This process can be manual, automated, or semi-automated based on jurisdictional capacity. Protocol should clearly outline the primary and secondary means of reaching a client and address confidentiality at the start of communication.
- Special considerations should be given to ensure culturally and linguistically appropriate communication.
- Protocols should be in place to provide services to people who are deaf or who have hearing loss.
- Depending on the source of the case report, information for locating a client may be insufficient. Tips on additional resources that may be used to obtain missing locating information can be found in Appendix B. Every effort should be made to reach the client remotely before attempting in-person communication.
Operational questions to consider
- How can your jurisdiction incorporate existing or new technology into a case investigator’s workflow to expedite patient notification?
- What technological precautions can be taken to ensure the confidentiality of clients and case investigators?
- What process will be followed when the client is a minor? Review jurisdiction-specific laws and consult with legal counsel if uncertain.
- When is in-person notification needed? Case investigators expected to perform in person notification need appropriate training on infection prevention and control practices and must obtain any necessary PPE prior to conducting in-person activities.
- How will positive test notifications be handled in congregate facilities (e.g., correctional facilities, homeless shelters, skilled nursing facilities, assisted care facilities, mental health facilities, various workplaces) where a positive test has implications for the client, other residents, staff, and visitors?
- How will investigations be handled for clients who are hospitalized and unable to be interviewed or deceased?
- What are local policies regarding interviewing of surrogates/proxies?
Step 3: Case interview
- Every effort should be made to interview the client by telephone or video conference instead of in-person. For in-person interviews, guidance on recommended infection prevention and control practices at a home or non-home residential setting can be found on CDC’s Evaluating PUIs Residential page.
- Clients in special populations and/or congregate settings may require additional considerations and should be triaged and assigned to a special infection control team, if available. See Outbreak Investigations for additional information.
- Appendix C includes critical data elements that can be incorporated into a jurisdiction’s paper form or electronic system used to elicit detailed information about a client’s close contacts and activity history, including any household contacts during self-isolation.
- Key Information to Collect During a Case Interview provides a roadmap for the case interview and identifies critical information to be collected during each part of an interview.
- Talking with the Patient – A Case Investigator’s Guide to COVID-19 focuses on communication strategies for case interviews and provides suggested language for each topic area covered in an interview.
Operational questions to consider
- If the client needs to be interviewed via an interpreter, how will those services be accessed?
- What steps will be taken if the patient is unwilling to communicate remotely (e.g., phone, video conference)?
- What procedures will be established to interview clients in correctional facilities? Hospitalized patients? Minors?
- What procedures will be established to locate and interview people experiencing homelessness?
Step 3a: Monitoring and isolation instructions
- Clients with probable or confirmed COVID-19 should be advised to self-isolate immediately, if they are not doing so already. Self-isolation is recommended for people with probable or confirmed COVID-19 who have mild illness and are able to recover at home.
- It should be made clear to the client whether the isolation instructions are voluntary or mandatory, as determined by state or local public health authorities.
- Advise clients to cancel or postpone plans that involve social gatherings, vacations or other planned travel until cleared for these activities by public health authorities.
- Local and state health departments may request federal public health travel restrictions, which prevent listed travelers from boarding commercial airplanes and trigger public health notification if they enter the United States by land or sea, to support state- or local-mandated isolation for infected individuals. Support with federal public health travel restrictions may be requested by public health partners by contacting the CDC quarantine station with jurisdiction for the area.
- If needed, jurisdictions should refer clients for social support services (for example, food, childcare, housing, and other services) to help encourage clients to stay at home and comply with isolation.
- If clients refuse to comply voluntarily with self-isolation instructions, jurisdictions should consider what options (e.g., legal order for isolation) are available to them under relevant state or local legal authority.
- The client should be informed of COVID-19 symptoms to monitor for and be instructed to get medical attention immediately if he/she experiences any emergency warning signs, such as trouble breathing. Clients with no primary healthcare provider will need linkage to telemedicine or phone consultation.
- The client should also be informed of ways to prevent infection among those living in their household.
- Additional isolation guidance should be reviewed with the client and instructional materials provided. Sample materials can be found on the CDC website:
- All instructions should be provided in a client’s primary language.
Operational questions to consider
- Under what circumstances will isolation be mandatory (under public health orders) as opposed to voluntary? How will this distinction be made clear to a patient?
- How will clients be monitored for isolation compliance?
- In the event that self-isolation is not feasible, what alternative supports exist, and/or what risk-reduction measures can be taken?
Step 3b: Assessing self-isolation support needs
Emphasis should be placed on helping clients identify any need for social support during self-isolation.
Isolation of clients with a diagnosis of COVID-19 prevents transmission to others and is critical to the success of any case investigation and contact tracing efforts. For most clients diagnosed with COVID-19 (i.e., those in an outpatient setting who are medically stable or discharged home following diagnosis at hospital), self-isolation can take place at home. If possible, clients should be asked to voluntarily stay home, monitor themselves for symptoms, and maintain social distance from others. The timeframe for self-isolation varies by case but, in general, people should isolate until the risk of secondary transmission is considered low. See Box 3 for specific instructions. Adherence to self-isolation instructions mainly depends on the clients’ needs and individual living situations, as well as on the support provided by the case investigation and contact tracing team.
Self-isolation requires that clients remain separate from others in the home, staying in a specific room away from other people and pets, and ideally with access to a separate bathroom. First and foremost, a case investigator should assess a patient’s ability to self-isolate in a safe environment that provides access to a private room and bathroom, as well as access to adequate food and water, among other considerations. For a portion of the U.S. population, self-isolation at home will be a challenge. It may be particularly difficult for some of the most vulnerable populations. Considerations must also be made for clients who express fear of abuse or violence if they must self-isolate at home. Additionally, some clients (e.g., single parents, nursing mothers, parents with children and toddlers, and other primary caregivers) may face other challenges, such as childcare or dependent adult care, that may affect the ability to self-isolate. Social services, housing and other supportive services will be needed for those who are unable to separate themselves from others in their current living situation. See Support Services for further considerations.
Clients will also need to be supported with health coaching to ensure daily monitoring of temperature and COVID-19 symptoms and have access to clinical services for medical concerns. Coordination of access to telehealth services, which may include remote access to non-clinical services, may be needed for clients without virtual access to a primary care provider. Reminding clients about the emergency warning signs and contact information for healthcare providers is imperative to ensure early medical management in the event that they develop new symptoms, or their symptoms worsen.
All clients with a confirmed or probable diagnosis of COVID-19 who are entering self-isolation in a non-healthcare setting ideally would be provided a COVID-19 kit with the following resources:*
- Washable cloth face covering
- Gloves
- Digital thermometer
- Alcohol-based hand sanitizer with at least 60% alcohol, soap, EPA-registered household disinfectantexternal icon
- COVID-19 health education materials (translated into the appropriate language)
- Instructions for cleaning and disinfecting your home for those sharing space with others
- A hotline/warmline to address any support needs during the self-isolation period, including medical, mental, and behavioral support
*The composition of the COVID-19 kit will depend on the jurisdiction’s resources.
Operational questions to consider
- Are there other resources that your jurisdiction can share to provide health advice and answer questions (e.g., mobile app, CDC Coronavirus Symptom Self-Checker, CDC-INFO)?
- Who can your jurisdiction partner with to provide other services to support clients during self-isolation?
Step 3c: Eliciting contacts
Identify close contacts
- Contact elicitation is a voluntary and critical part of the case interview.
- The case investigator can use information from any reports received by the health department, along with the patient’s symptom history gathered earlier in the case interview, to determine the contact elicitation window (the timeframe when the patient was infectious and not under isolation). See Box 2 below for additional guidance on determining the contact elicitation window.
- A close contact is defined as someone who was less than 6 feet away from an infected person for a cumulative total of 15 minutes or more over a 24-hour period.
- It will be important that the case investigator clearly explain why close contacts are being elicited and assure the patient that their identity will not be disclosed to any close contacts that they identify.
- The trust and rapport built earlier in the case interview, combined with open-ended and probing questions, will help facilitate the contact elicitation portion of the interview.
- Information to be gathered for each close contact can be found in the Contact Elicitation Investigation data elements table in Appendix C and includes the contact’s name and locating information, the setting of the exposure, contact’s work setting and occupation, and any underlying health conditions or other risk factors the contact may have (if known by the patient).
- In communities near international land borders, specific interview questions should be asked to identify relevant contacts across the border.
- The case investigator should also confirm the best way to reach the patient for any follow-up discussion.
- Proxy interviews are essential when the patient cannot be interviewed (e.g., patient is deceased, intubated, unconscious, a minor, cognitively impaired). Key proxy interviewees are those likely to know the patient’s practices, habits, and behaviors. However, because proxy interviews jeopardize patient confidentiality, jurisdictions should establish clear guidelines for these interviews that recognize the challenge of maintaining confidentiality.
Box 2. Determining the contact elicitation window
In order to elicit contacts from a client with confirmed or probable COVID-19, a case investigator will first need to determine the appropriate contact elicitation window. An assessment of the client’s COVID-19 symptoms or positive test date (based on date of specimen collection) if they do not have symptoms, will help identify their infectious period. Building on that information, the contact elicitation window is the timeframe when the client was infectious and not under isolation. If there are additional close contacts during isolation (such as household contacts), those close contacts should also be elicited.
Client with Confirmed or Probable COVID-19
When interviewing a person with confirmed or suspected COVID-19, a case investigator should elicit all close contacts from 2 days prior to onset of any symptoms, or from the date of the positive test (based on specimen collection date) if they do not have symptoms, through the beginning of isolation. People who are exposed to someone with COVID-19 after they completed at least 5 days of isolation are not considered close contacts.
Start date: 2 days before symptom* onset or date of positive test (based on specimen collection date)
End date: Beginning of isolation period OR until discontinuation of home isolation (to elicit household contacts of clients recovering at home)
*All possible symptoms should be considered, with particular attention to those that may be mild and/or nonspecific (e.g., fatigue, muscle pain) and those less common.
Operational questions to consider
- How can your jurisdiction use technology to facilitate contact elicitation (e.g., asking about contacts that are stored in a client’s phone)?
- What types of data tools would help increase efficiency?
- How will case investigators document and transfer the list of contacts to the contract tracer?
- Will clients be asked to notify household contacts or close contacts themselves? How will client-notified contacts be managed and dispositioned?
- If an employer knows the identity of an employee diagnosed with COVID-19, how can a list of close contacts from the worksite best be gathered?
Step 4: Case follow-up & medical monitoring
- The initial case interview covers a great deal of material, which can be overwhelming for a client.
- In some instances, the case investigator may need to follow up with the client to clarify details from the
conversation including:
-
- Onset of symptoms, particularly the nonspecific symptoms (e.g., fatigue, muscle pain);
- Further exploration of occupation and interactions in the workplace or last day at work;
- Transportation to and from work, social and recreational activities;
- Additional locating information for close contacts or additional contacts from their self-isolation period;
- Home, family, and other factors that could affect their compliance with self-isolation.
- Ideally, all clients diagnosed with COVID-19 will be monitored using real-time communication methods (e.g., telephone call, video conferencing) to share daily reports on their temperature and COVID-19 symptoms throughout the length of their self-isolation.
- Prioritizing which clients to monitor closely and which may be able to adequately self-monitor should be determined in the context of existing resources. In some instances, clients with underlying health conditions and other special circumstances (such as pregnancy) may present complex medical challenges. While these may not require hospitalization, these clients may need in-home medical monitoring by a healthcare provider until their COVID-19 symptoms resolve.
- If a jurisdiction’s resources do not allow for active daily monitoring, clients will be asked to self-monitor and communicate remotely (e.g., email, recorded video, telephone message, text, monitoring apps) to notify public health authorities of their health status and promptly communicate any new symptoms or symptoms of increasing severity.
- For those individuals self-monitoring and sharing reports remotely, reports must be received by the agreed upon time each day, and protocol must address follow-up actions for clients who do not report out.
Operational questions to consider
- What types of tools and schedules will be used for medical monitoring?
- Which staff in the jurisdiction will conduct medical monitoring? Will certain cases be delegated to a staff member with clinical expertise (e.g., complex or high-risk cases)?
- What social support is necessary for a client to maintain self-isolation? What support may a client’s family need?
- What criteria will your jurisdiction use to refer clients to healthcare or emergency services?
- What steps will be taken for self-monitoring clients who do not comply with reporting requirements? How intensive will the outreach be (e.g., same-day home visit)?
- How will appropriate privacy protections be maintained?
Step 5: Additional case follow-up
- Additional follow-up may be needed for clients with COVID-19 who are transitioning from one facility to another—for example, from a hospital to a long-term care facility or to home isolation. Care coordination plans should be put in place to maintain proper infection control and isolation procedures.
- Additional coordination will also be necessary to support clients with COVID-19 who are discharged from a correctional facility (e.g., prisons, jails, youth detention centers). These individuals will be transitioning to self-isolation in their home communities and will need assessment for social supports to ensure adequate housing, food, and medical care throughout the remainder of their self-isolation.
- Transitional case management plans are incredibly important to ensure continuity of care for clients with COVID-19 and protect the community from further transmission.
Step 6: Discontinuation of isolation
Duration of isolation depends on many factors, including symptom status, illness severity and setting (for example, correctional facilities, shelters, or healthcare facilities). Case investigators should refer to current CDC guidance on isolation guidance COVID-19 Quarantine and Isolation when providing recommendations to people with COVID-19.