Aquatics FAQs
Recommendations for Fully Vaccinated People
COVID-19 Homepage
Interim Guidance for Antigen Testing for SARS-CoV-2
Summary of Recent Changes
Key Points
- This interim guidance is intended for healthcare providers who order antigen tests, receive antigen test results, or perform point-of-care testing, as well as for laboratory professionals who perform antigen testing in a laboratory setting or at the point of care and report those results.
- The purpose of this interim technical guidance is to support effective clinical and public health use of antigen tests for different testing situations.
- This guidance applies to all clinical and consumer uses of antigen tests and is not specific to any particular age group.
- This guidance incorporates considerations for fully vaccinated people and should be used in conjunction with CDC’s Interim Public Health Recommendations for Fully Vaccinated People.
- General Guidance
- Regulatory Requirements for Using Antigen Tests for SARS-CoV-2
- Performance of Antigen Tests for SARS-CoV-2
- Processing of Antigen Tests for SARS-CoV-2
- Evaluating the Results of Antigen Testing for SARS-CoV-2
- Using Antigen Tests for SARS-CoV-2 in Congregate Living Settings
- Using Antigen Tests for SARS-CoV-2 in Community Settings
- Confirmatory Testing When Using Antigen Tests for SARS-CoV-2
- Serial Testing When Using Antigen Tests for SARS-CoV-2
- Reporting Antigen Test Results for SARS-CoV-2 to Health Departments and Patients
Antigen Testing for SARS-CoV-2
Antigen tests are commonly used in the diagnosis of respiratory pathogens, including influenza viruses and respiratory syncytial virus. The U.S. Food and Drug Administration (FDA) has granted emergency use authorization (EUA) for antigen tests that can identify SARS-CoV-2. See FDA’s list of In Vitro Diagnostics EUAsexternal icon.
Antigen tests are immunoassays that detect the presence of a specific viral antigen, which implies current viral infection. Antigen tests are currently authorized to be performed on nasopharyngeal or nasal swab specimens placed directly into the assay’s extraction buffer or reagent. The currently authorized antigen tests include point-of-care, laboratory-based, and self-tests, and they are applicable to people of any age. See Table 1 for additional information about antigen tests.
Antigen tests are relatively inexpensive, and most can be used at the point of care. Most of the currently authorized tests return results in approximately 15–30 minutes. Antigen tests for SARS-CoV-2 are generally less sensitive than real-time reverse transcription polymerase chain reaction (RT-PCR) and other nucleic acid amplification tests (NAATs) for detecting the presence of viral nucleic acid. However, NAATs can remain positive for weeks to months after initial infection and can detect levels of viral nucleic acid even when virus cannot be cultured, suggesting that the presence of viral nucleic acid may not always indicate contagiousness.
Proper interpretation of both antigen test results and NAATs (when indicated) is important for accurate clinical management of patients or people with suspected COVID-19, or for identification of infected people when used for screening.
The clinical performance of diagnostic tests largely depends on the circumstances in which they are used. Both antigen tests and NAATs perform best if the person is tested when their viral load is generally highest. Because antigen tests perform best in symptomatic people and within a certain number of days since symptom onset, antigen tests are used frequently on people who are symptomatic. Antigen tests also may be informative in diagnostic testing situations in which the person has a known exposure to a person with COVID-19.
Accumulation of data on the performance of antigen tests in different situations has helped guide the use of these tests as screening tests in asymptomatic people to detect or exclude SARS-CoV-2 infection. See FDA’s Recommendations for healthcare providers using SARS-CoV-2 diagnostic tests for screening asymptomatic individuals for COVID-19external icon. Also see information from the Centers for Medicare & Medicaid Services (CMS) on Updated CLIA SARS-CoV-2 Molecular and Antigen Point of Care Test Enforcement Discretionexternal icon.
Antigen tests have been used for screening testing in high-risk congregate housing settings, such as nursing homes, in which repeat testing has quickly identified people with COVID-19, informing infection prevention and control measures, thus preventing transmission. In this case, and where rapid test turnaround time is critical, there is value in providing immediate results with antigen tests, even though they may have lower sensitivity than NAATs.
Healthcare providers and public health practitioners should understand test performance characteristics to recognize potentially false negative or false positive test results and to guide additional confirmatory testing and management of the patient or person. Laboratory and testing professionals who perform antigen tests should understand the factors that affect the accuracy of antigen testing, as described in this guidance. Healthcare providers, laboratory and testing professionals, and public health practitioners should also understand the differences among diagnostic, screening, and surveillance testing. See CDC’s Overview of Testing for SARS-CoV-2, and Testing Strategies for SARS-CoV-2. Also see FDA’s FAQs on Testing for SARS-CoV-2external icon.
This guidance supplements and is consistent with CDC’s Overview of Testing for SARS-CoV-2 and SARS-CoV-2 Point-of-Care and Rapid Testing guidance. CDC has also published guidance on SARS-CoV-2 Antigen Testing in Long Term Care Facilities, Interim Guidance for SARS-CoV-2 Testing in Correctional and Detention Facilities, Interim Guidance for SARS-CoV-2 Testing in Homeless Shelters and Encampments, and Operating Schools During COVID-19: CDC’s Considerations.
Regulatory Requirements for Using Antigen Tests for SARS-CoV-2
FDA regulates in vitro diagnostic devices and has provided recommendations and information regarding EUA requests for COVID-19 diagnostic tests in the Policy for Coronavirus Disease-2019 Tests During the Public Health Emergency (Revised) (“Policy for COVID-19 Tests”)external icon and the EUA templates referenced in that policy. COVID-19 tests and test systems used for diagnostic or screening testing, including those for antigen testing, must have received an EUA from FDA or be offered under the policies in FDA’s Policy for COVID-19 Testsexternal icon. Every antigen test for SARS-CoV-2 authorized for use by FDA is included on FDA’s list of In Vitro Diagnostics EUAsexternal icon. The intended use of each test, available in the Instructions for Use and in the Letter of Authorization, defines the population in which the test is intended to be used, the acceptable specimen types, and how the results should be used.
Laboratory and testing professionals who conduct diagnostic or screening testing for SARS-CoV-2 with antigen tests must also comply with Clinical Laboratory Improvement Amendments (CLIA) regulations. Any laboratory or testing site that intends to report patient-specific test results to a person or healthcare provider must first obtain a CLIA certificate and meet all requirements to perform that testing. For more information, see CMS’ How to Obtain a CLIA Certificateexternal icon. CMS has provided additional information on Enforcement discretion for the use of SARS-CoV-2 point-of-care testing on asymptomatic individualsexternal icon.
Performance of Antigen Tests for SARS-CoV-2
It is important for healthcare providers and testing personnel to understand the performance characteristics, including sensitivity, specificity, and positive and negative predictive values, of the particular antigen test being used, and to follow the manufacturer’s instructions for use, which summarize performance characteristics. See FDA’s In Vitro Diagnostics EUAsexternal icon for detailed information about specific authorized tests.
The “gold standard” for clinical diagnostic detection of SARS-CoV-2 remains laboratory-based (moderate- and high-complexity) NAATs. Thus, it may be necessary to confirm an antigen test result with a laboratory-based NAAT, especially if the result of the antigen test is inconsistent with the clinical context. Table 1 summarizes the differences between NAATs and antigen tests. Clinical performance of NAATs and antigen tests may differ from clinical utility when considering issues of test availability, quality of specimen collection and transport, and turnaround times of results. Based on their instructions for use, some point-of-care NAATs may not be used for confirmatory testing. NAATs that generate presumptive results are not appropriate for use in confirmatory testing.
The sensitivity of antigen tests varies but is generally lower than most laboratory-based NAATs. The antigen level in specimens collected either before symptom onset, or late in the course of infection, may be below the tests’ limit of detection. This may result in a negative antigen test result, while a more sensitive test, such as most NAATs, may return a positive result. Studiesexternal icon have shown that antigen tests have comparable sensitivity to laboratory-based NAATs when viral load in the specimen is high and the person is likely to be most contagious.
The specificity of antigen tests is generally as high as most NAATs, which means that false positive test results are unlikely when an antigen test is used according to the manufacturer’s instructions. Despite the high specificity of antigen tests, false positive results will occur, especially when used in communities where the prevalence of infection is low – a circumstance that is true for all in vitro diagnostic tests. In general, for all diagnostic tests, the lower the prevalence of infection in the community, the higher the proportion of false positive test results.
Positive and negative predictive values of all in vitro diagnostic tests (e.g., NAAT and antigen tests) vary depending upon the pretest probability. Pretest probability considers both the prevalence of the target infection in the population that is being tested as well as the clinical context of the individual being tested. If the prevalence of infection in the community is high, and the person being tested is symptomatic, then the pretest probability is generally considered high. If the prevalence of infection in the community is low, and the person being tested is asymptomatic and has not had any known contact to a person with COVID-19, then the pretest probability is generally considered low. See CDC’s Interpreting Results of Diagnostic Tests for additional information on the relationship between pretest probability and the likelihood of positive and negative predictive values.
To help estimate pretest probability, CDC recommends that laboratory and testing professionals who perform antigen testing determine infection prevalence based on a rolling average of the positivity rate of their own SARS-CoV-2 testing over the previous 7–10 days. Alternatively, state health departments generally publish COVID-19 data on testing positivity rates and case rates for their communities.
Processing of Antigen Tests for SARS-CoV-2
The Conditions of Authorization in the antigen EUAs specify that CLIA-certified laboratories and testing sites are to follow the manufacturer’s instructions for use, typically found in the package insert, when performing the test and reading test results. The authorized instructions for use for each test can also be found at FDA’s In Vitro Diagnostics EUAsexternal icon.
For example, the performance of antigen tests can be affected if the test components are not stored and handled properly. They should never be frozen and should always be allowed to reach room temperature (15-30°C) before use. The package insert for these tests includes instructions for handling of the test cartridge/card, such as ensuring it remains in its sealed pouch until immediately before use.
The package insert for antigen tests also includes instructions about how to read the test results, including the appropriate time to read the results and whether the results should be interpreted visually or with an instrument analyzer. Reading the test before or after the specified time could result in false positive or false negative test results.
Processing multiple specimens successively or in batch mode may increase the risk of contamination and may make it more challenging to ensure that each specimen is incubated for the correct amount of time before the result is read. Refer to the package insert for the correct incubation time for that test, and then monitor and ensure proper timing for each specimen during testing and when reading results.
All testing for SARS-CoV-2, including antigen testing, depends on the integrity of the specimen, which is affected by procedures for both specimen collection and handling. Improper specimen collection, such as swabbing the nostril too quickly, may cause insufficient specimen collection, resulting in limited amounts of viral genetic or antigenic material for detection. Time from specimen collection to testing should be minimized, and the temperature of the specimen during this time must be controlled. See CDC’s Interim Guidelines for Collecting, Handling, and Testing Clinical Specimens for COVID-19.
Quality assurance procedures should be followed to prevent cross-contamination and inaccurate test results. For example, users should follow the manufacturer’s instructions, as well as state and local guidance, for when and how often to perform testing on control specimens. If antigen testing returns multiple unexpected positive results, it may be appropriate to stop testing patient specimens, review all procedures, clean all surfaces, change gloves, and run control specimens before restarting the testing of patient specimens. In such circumstances, confirmatory testing should be considered for people who received unexpected results, regardless of pretest probabilities.
Clean work surfaces and equipment regularly (daily or as often as needed) with soap or detergent. If regular disinfection is needed, use an EPA-approved disinfectant for SARS-CoV-2, following the manufacturer’s recommendations for use, such as dilution, contact time, and safe handling. See EPA’s List of Disinfectants for COVID-19external icon. Gloves should be changed before collecting, handling, and processing a new specimen in the antigen test system. Failing to change gloves can increase the risk of cross-contamination and false antigen test results. See CDC’s guidance on Point-of-Care Testing, and Interim Laboratory Biosafety Guidelines for Handling and Processing Specimens Associated with Coronavirus Disease 2019 (COVID-19).
Some antigen tests have explored the use of viral transport medium (VTM) during specimen collection, but the use of VTM may cause false test results from either cross-reactivity with the capture antibodies or dilution of the specimen that decreases the sensitivity of the test. Laboratories and testing sites should refer to the instructions for use and the package insert that are specific for the test that they are using regarding the use of VTM.
Also see FDA’s Letter to Clinical Laboratory Staff and Health Care Providersexternal icon on the potential for false positive results with antigen tests, and CDC’s guidance on Point-of-Care Testing.
Evaluating the Results of Antigen Testing for SARS-CoV-2
Evaluating the results of an antigen test for SARS-CoV-2 depends primarily on the clinical and epidemiological context of the person who has been tested (e.g., symptoms, exposure to others with COVID-19, vaccination status, previous infection status, or setting in which they live). For additional details on testing recommendations see guidance for fully vaccinated people. A particularly important aspect of epidemiological context is whether the person to be tested is a resident or an employee of a congregate living facility. In addition, evaluating the results of an antigen test for SARS-CoV-2 should consider the performance characteristics (e.g., sensitivity, specificity) and the instructions for use of the FDA-authorized test, and the prevalence of SARS-CoV-2 infection in that particular community (percent positivity rate over the previous 7–10 days or the number of cases in the community relative to the population size).
The evaluation of an antigen test result should consider whether the person has experienced symptoms, and if so for how long. Generally, healthcare providers can rely upon a positive antigen test result for a symptomatic patient because the specificity of current FDA-authorized antigen tests is high.
The sensitivity of current FDA-authorized antigen tests varies, and thus negative diagnostic testing results should be handled depending on the circumstances. In most circumstances, the manufacturers’ instructions for use of antigen tests indicate that negative test results should be considered “presumptive,” meaning that they are preliminary results. See FDA’s In Vitro Diagnostics EUAsexternal icon.
It may be appropriate to confirm antigen test results with a laboratory-based NAAT. For confirmatory testing, CDC recommends using a laboratory-based NAAT that has been evaluated against the FDA reference panel for analytical sensitivity. See FDA’s SARS-CoV-2 Reference Panel Comparative Dataexternal icon. NAATs that generate presumptive results are not appropriate for use in confirmatory testing.
CDC has developed two general antigen testing algorithms to accommodate two broad categories of use for antigen tests. CDC recommends following one of these two antigen testing algorithms to determine when confirmatory testing is recommended.
The first algorithm is designed for those who live in congregate settings, such as long-term care facilities, correctional and detention facilities, homeless shelters, and other group shelters. In these settings, correct case identification is particularly important because of the need to group isolated people together or in close proximity, so false positive test results can have significant negative consequences. See Figure 1, also available as a PDF. This algorithm is not designed for employees of congregate living facilities, who can quarantine and isolate outside of the facility if necessary.
The second algorithm is designed for community testing among people who do not live in congregate settings. The primary objective of this testing is to reduce the transmission of SARS-CoV-2 in the community, where there are concerns for introduction and widespread transmission, by quickly identifying and isolating people who are infected. See Figure 2, also available as a PDF.
Using Antigen Tests for SARS-CoV-2 in Congregate Living Settings
Figure 1. Antigen Test Algorithm for Congregate Living Settings
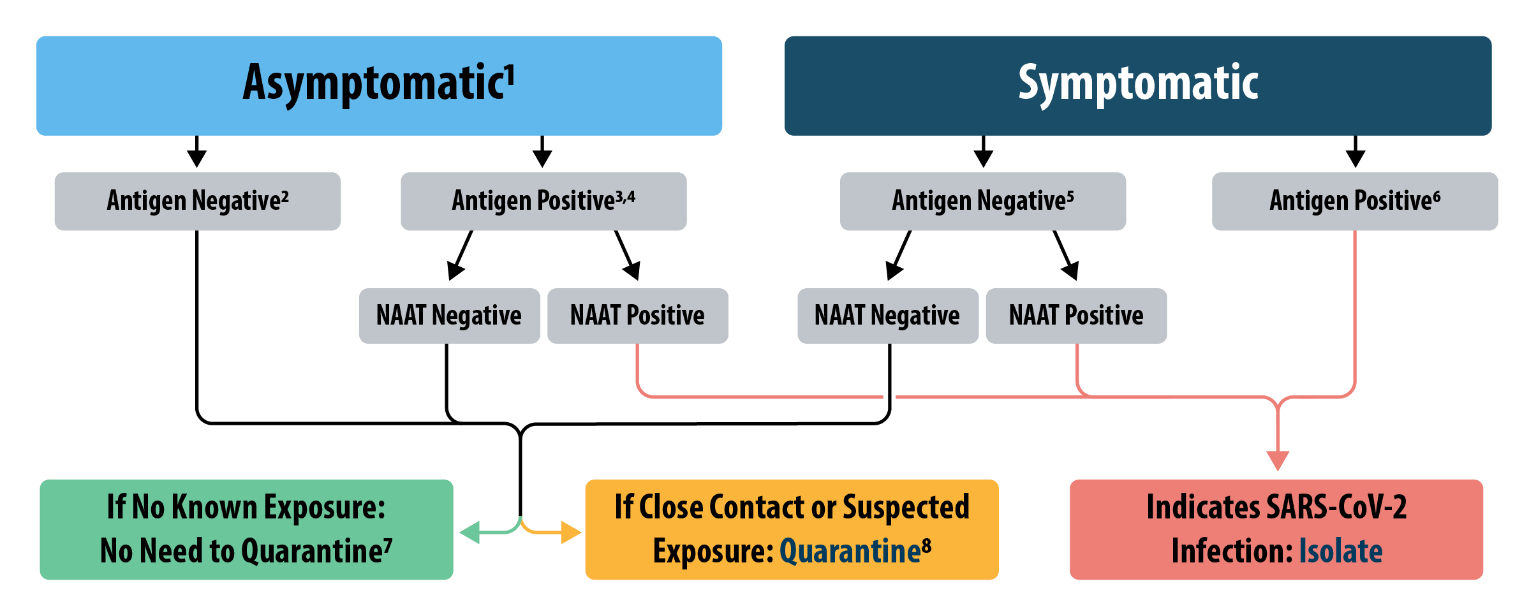
1 Asymptomatic people who are fully vaccinated should follow CDC’s guidance on testing for fully vaccinated people. Asymptomatic people who have had a SARS-CoV-2 infection in the last 3 months should follow CDC’s guidance on testing for those within 90 days of their initial infection. For those who are traveling or have recently traveled, refer to CDC’s guidance for domestic and international travel during the COVID-19 pandemic.
2 This antigen negative may need confirmatory testing if the person has a high likelihood of SARS-CoV-2 infection (e.g., the person has had close contact or suspected exposure to a person with COVID-19 within the last 14 days and the person is not fully vaccinated and has not had a SARS-CoV-2 infection in the last 3 months). Also see Options to Reduce Quarantine.
3 This antigen positive may not need confirmatory testing if the person has a high likelihood of SARS-CoV-2 infection (see above).
4 If resources and access to confirmatory laboratory-based NAATs are limited, and the prevalence of infection is relatively high, congregate facilities may consider performing a second antigen test within 8 hours of the first positive antigen result. If the result is concordant and the second test is positive, the person should follow guidance for isolation. If the result is discordant and the second test is negative, then the person should have a confirmatory NAAT.
5 This antigen negative may not need confirmatory testing if the person has a low likelihood of SARS-CoV-2 infection (e.g., the person has had no known or suspected exposure to a person with COVID-19 within the last 14 days or is fully vaccinated or has had a SARS-CoV-2 infection in the last 3 months).
6 This antigen positive may need confirmatory testing if the person has a low likelihood of SARS-CoV-2 infection (see above) or if the facility has had more than one unexpected positive test result that day.
7 For those who are traveling or have recently traveled, refer to CDC’s guidance for domestic and international travel during the COVID-19 pandemic.
8 People who have had close contact with a person with COVID-19 within the last 14 days should follow CDC’s guidance for quarantine. If there is an outbreak in the facility, serial testing should be performed every 3-7 days until there are no new cases for 14 days. People in facilities with an outbreak should follow site-specific public health measures, such as transmission-based precautions. For guidance on the use of antigen tests in ending quarantine, see CDC’s Options to Reduce Quarantine, Recommendations to Prevent SARS-CoV-2 Spread in Nursing Homes, Recommendations for Quarantine Duration in Correctional and Detention Facilities, and Interim Guidance for Homeless Shelters and Encampments.
Testing a symptomatic person in a congregate living setting
When testing a person who resides in a congregate living setting who has symptoms compatible with COVID-19, the healthcare provider generally can interpret a positive antigen test to indicate that the person is infected with SARS-CoV-2; this person should follow CDC’s guidance for isolation. In healthcare settings, infection prevention and control practices for caring for a person with COVID-19 should be followed until their isolation is discontinued. However, if the person who has received a positive antigen test result is fully vaccinated, the healthcare provider should inform public health authorities. When possible, a separate specimen should be collected and sent to a laboratory for viral sequencing for public health purposes.
A positive antigen test result for a symptomatic person may need confirmatory testing if the person has a low likelihood of SARS-CoV-2 infection. For example, a low likelihood of SARS-CoV-2 infection would be a person who has not had a known or suspected exposure to a person with COVID-19 within the last 14 days or is fully vaccinated or has had a SARS-CoV-2 infection in the last 3 months. If the congregate living facility has had more than one unexpected positive test result that day, then that positive antigen test result may need confirmatory testing.
A negative antigen test result for a symptomatic person should be confirmed with a laboratory-based NAAT. A negative antigen result for a symptomatic person may not need confirmatory testing if the person has a low likelihood of SARS-CoV-2 infection (see above). A symptomatic person who has received a negative antigen test result and then a positive confirmatory NAAT should follow CDC’s guidance for isolation.
A symptomatic person who has received a negative antigen test result and then a negative confirmatory NAAT but has had close contact with a person with COVID-19 within the last 14 days should follow CDC’s guidance for quarantine, which may include retesting 5-7 days after last known exposure. A symptomatic person who has received a negative antigen test result and then a negative confirmatory NAAT but has a suspected exposure (such as an outbreak in the facility) should follow site-specific public health measures, such as quarantine and transmission-based precautions and should be serially tested every 3-7 days until there are no new cases for 14 days. For guidance on the use of antigen tests in ending quarantine, see CDC’s Options to Reduce Quarantine, Recommendations to Prevent SARS-CoV-2 Spread in Nursing Homes, Recommendations for Quarantine Duration in Correctional and Detention Facilities, and Interim Guidance for Homeless Shelters and Encampments.
Testing an asymptomatic person in a congregate living setting
When testing an asymptomatic person for COVID-19, the healthcare provider should follow a positive antigen test result with a laboratory-based confirmatory NAAT. If an asymptomatic person receives a positive antigen test result and then a positive confirmatory NAAT result, they should follow CDC’s guidance for isolation. A positive antigen test result from an asymptomatic person may not need confirmatory testing if the person has a high likelihood of SARS-CoV-2 infection. For example, a high likelihood of SARS-CoV-2 infection would be a person who has had close contact with or suspected exposure to a person with COVID-19 within the last 14 days and is not fully vaccinated and has not had a SARS-CoV-2 infection in the last 3 months.
When testing an asymptomatic person for COVID-19, the healthcare provider generally can interpret a negative antigen result to indicate that a SARS-CoV-2 infection is not present. However, a negative antigen test result may need confirmatory testing if that asymptomatic person has a high likelihood of SARS-CoV-2 infection (see above).
An asymptomatic person who has received a negative antigen test result, or a positive antigen test result and then a negative confirmatory NAAT, should follow CDC’s guidance for quarantine if they have had close contact with or suspected exposure to a person with COVID-19 within the last 14 days. If that same person has not had any known exposure to COVID-19 within the last 14 days, then they do not need to quarantine.
If there is an outbreak in the facility (one or more cases of COVID-19), everyone is suspected to have exposure, therefore, serial testing should be performed every 3-7 days until there are no new cases for 14 days. Serial antigen testing should be more frequent than serial NAAT testing. For guidance on the use of antigen tests in ending quarantine, see CDC’s Options to Reduce Quarantine, Recommendations to Prevent SARS-CoV-2 Spread in Nursing Homes, Recommendations for Quarantine Duration in Correctional and Detention Facilities, and Interim Guidance for Homeless Shelters and Encampments. Those who plan to travel or have recently traveled should refer to CDC’s guidance for domestic and international travel during the COVID-19 pandemic.
Using Antigen Tests for SARS-CoV-2 in Community Settings
Figure 2. Antigen Test Algorithm for Community Settings
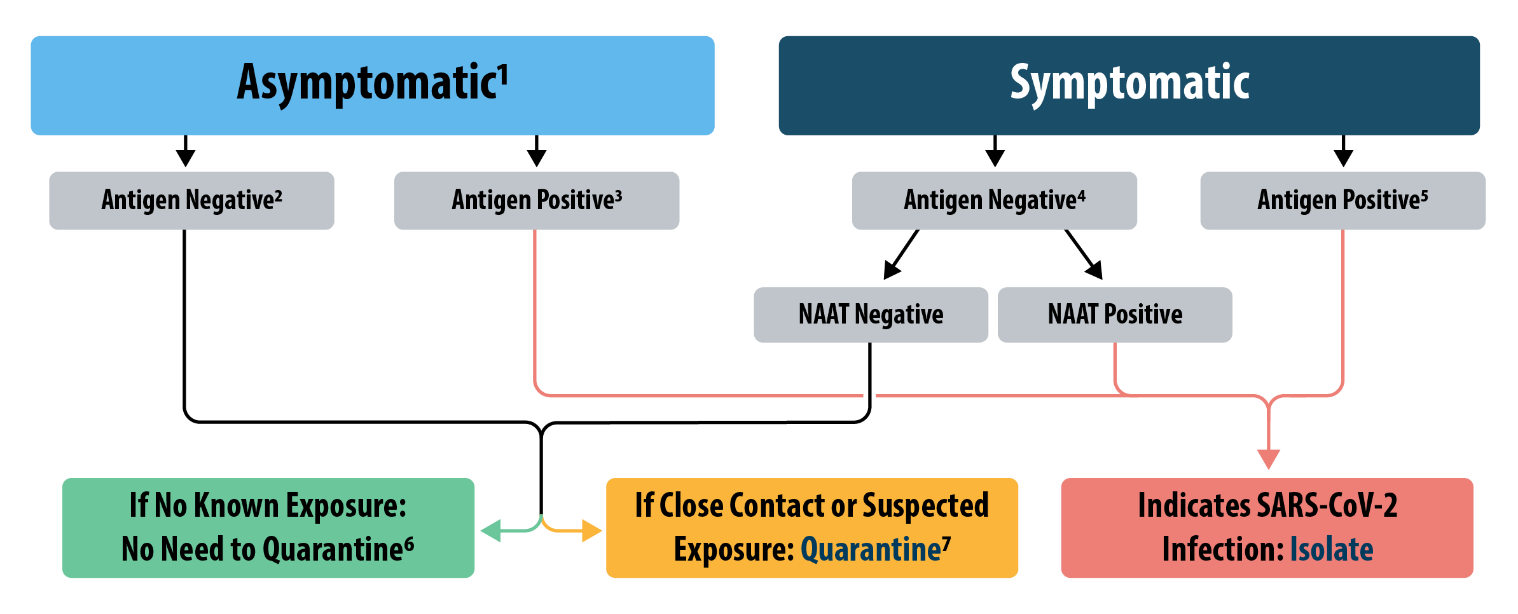
1 Asymptomatic people who are fully vaccinated should follow CDC’s guidance on testing for fully vaccinated people. Asymptomatic people who have had a SARS-CoV-2 infection in the last 3 months should follow CDC’s guidance on testing for those within 90 days of their initial infection. For those who are traveling or have recently traveled, please refer to CDC’s guidance for domestic and international travel during the COVID-19 pandemic.
2 This antigen negative may need confirmatory testing if the person has a high likelihood of SARS-CoV-2 infection (e.g., the person has had close contact with or suspected exposure to a person with COVID-19 within the last 14 days and the person is not fully vaccinated and has not had a SARS-CoV-2 infection in the last 3 months). Also see Options to Reduce Quarantine.
3 This antigen positive may need confirmatory testing if the person has a low likelihood of SARS-CoV-2 infection (e.g., the person has had no known or suspected exposure to a person with COVID-19 within the last 14 days or is fully vaccinated or has had a SARS-CoV-2 infection in the last 3 months).
4 This antigen negative may not need confirmatory testing if the person has a low likelihood of SARS-CoV-2 infection (see above).
5 This antigen positive may need confirmatory testing if the person has a low likelihood of SARS-CoV-2 infection (see above).
6 For those who are traveling or have recently traveled, refer to CDC’s guidance for domestic and international travel during the COVID-19 pandemic.
7 Fully vaccinated people and those who have had a SARS-CoV-2 infection in the last 3 months do not need to quarantine. Others should consider serial antigen testing if they have had contact with a person who has COVID-19 within the last 14 days. For guidance on the use of antigen tests in ending quarantine, see CDC’s Options to Reduce Quarantine.
Testing a symptomatic person in a community setting
In a community setting, when testing a person who has symptoms compatible with COVID-19, the healthcare provider generally can interpret a positive antigen test to indicate that the person is infected with SARS-CoV-2; this person should follow CDC’s guidance for isolation. However, if the person who has received a positive antigen test result is fully vaccinated, the healthcare provider should inform the public health authorities. Ideally, a separate specimen would be collected and sent to a laboratory for viral sequencing for public health purposes.
A positive antigen test result for a symptomatic person may need confirmatory testing if the person has a low likelihood of SARS-CoV-2 infection. For example, a low likelihood of SARS-CoV-2 infection would be a person who has had no known exposure to a person with COVID-19 within the last 14 days or is fully vaccinated or has had a SARS-CoV-2 infection in the last 3 months.
A negative antigen test result for a symptomatic person should be confirmed with a laboratory-based NAAT. In this case, an alternative to confirmatory NAAT testing is serial antigen testing that is performed every 3–7 days for 14 days.
A negative antigen result for a symptomatic person may not need confirmatory testing if the person has a low likelihood of SARS-CoV-2 infection (see above).
A symptomatic person who has received a negative antigen test result and then a positive confirmatory NAAT should follow CDC’s guidance for isolation. A symptomatic person who has received a negative antigen test result and then a negative confirmatory NAAT should follow CDC’s guidance for quarantine if they have had close contact or suspected exposure to a person with COVID-19 within the last 14 days. If that same person has not had any known exposure to COVID-19, then they do not need to quarantine.
Testing an asymptomatic person in a community setting
Asymptomatic vaccinated people should follow CDC’s Interim Public Health Recommendations for Fully Vaccinated People and do not need to pursue testing in most cases. When testing an asymptomatic person in a community setting for COVID-19, the healthcare provider generally can interpret a positive antigen test to indicate that the person is infected with SARS-CoV-2; this person should follow CDC’s guidance for isolation. A positive antigen test result from an asymptomatic person may need confirmatory testing if the person has a low likelihood of SARS-CoV-2 infection. For example, a low likelihood of SARS-CoV-2 infection would be a person who has had no known exposure to a person with COVID-19 within the last 14 days or is fully vaccinated or has had a SARS-CoV-2 infection in the last 3 months.
When testing an asymptomatic person for COVID-19, the healthcare provider generally can interpret a negative antigen result to indicate that a SARS-CoV-2 infection is not present. However, a negative antigen test result may need confirmatory testing if that asymptomatic person has a high likelihood of SARS-CoV-2 infection. For example, a high likelihood of SARS-CoV-2 infection would be a person who has had close contact or suspected exposure to COVID-19 within the last 14 days and the person is not fully vaccinated and has not had a SARS-CoV-2 infection in the last 3 months.
An asymptomatic person who has received a negative antigen test result should follow CDC’s guidance for quarantine if they have had close contact or suspected exposure to a person with COVID-19 within the last 14 days; fully vaccinated people and those who have had a SARS-CoV-2 infection in the last 3 months do not need to quarantine. Those who are not fully vaccinated and have not had COVID-19 in the last 3 months should consider serial antigen testing if they have had contact with a person who has COVID-19 within the last 14 days. Serial antigen testing should be performed every 3–7 days for 14 days. For guidance on the use of antigen tests in ending quarantine, see CDC’s Options to Reduce Quarantine. Those who plan to travel or have recently traveled should refer to CDC’s guidance for domestic and international travel during the COVID-19 pandemic.
COVID-19 Viral Testing Tool
A tool to help healthcare providers quickly access the most relevant, actionable information to determine what type(s) of COVID-19 testing they should recommend. After test results are in, the tool can help interpret test results and guide next steps.
Confirmatory Testing When Using Antigen Tests for SARS-CoV-2
As the antigen testing algorithms indicate, confirmatory testing may be needed regardless of the symptom or exposure status of the person being tested. Confirmatory testing should take place as soon as possible after the antigen test, and not longer than 48 hours after the initial antigen testing. If more than 48 hours separate the two specimen collections, or if there have been opportunities for new exposures, a laboratory-based NAAT should be considered a separate test – not a confirmation of the earlier test. If the results are discordant between the antigen test and the confirmatory NAAT, in general the confirmatory test result should be interpreted as definitive for the purpose of clinical diagnosis.
CDC recommends laboratory-based NAATs for confirmatory testing. CDC does not recommend NAATs that use oral specimens (e.g., saliva) for confirmatory testing and instead suggests the use of specimens that are considered optimal for detection, such as nasopharyngeal, nasal mid-turbinate, and anterior nasal swabs. See CDC’s guidance for Nucleic Acid Amplification Tests (NAATs).
Several studies have documented persistent or intermittent detection of virus using RT-PCR after recovery; in these cases, the people did not seem to be infectious to others. Thus, if the person being tested has recently had COVID-19 and completed their period of isolation, it is possible for that person to receive a negative antigen test result and a positive confirmatory NAAT, potentially indicating a persistent detection of SARS-CoV-2 after recovery from COVID-19. For this reason, repeat testing after the initial diagnostic test is not recommended during the period of isolation or as a test of cure. See CDC’s Clinical Questions about COVID-19: Questions and Answers.
If confirmatory testing is not available, clinical discretion can determine whether to recommend that the patient isolate or quarantine. See CDC’s guidance on Testing in Nursing Homes, Quarantine and Isolation, Discontinuation of Isolation for Persons with COVID-19 Not in Healthcare Settings, Discontinuation of Transmission-Based Precautions of Patients in Healthcare Settings, Return to Work for Healthcare Personnel, Recommendations for Quarantine Duration in Correctional and Detention Facilities, and Operating Schools During COVID-19: CDC’s Considerations.
Serial Testing When Using Antigen Tests for SARS-CoV-2
Depending on the circumstances and setting, it may be useful to implement serial antigen testing for persons who receive a negative antigen test result. Serial antigen testing within a congregate living setting, such as a long-term care facility or a correctional or detention facility, could quickly identify someone with a SARS-CoV-2 infection and prevent further transmission. It may not be necessary to perform confirmatory testing with a NAAT when conducting serial antigen testing on those who have received a negative antigen test result.
Modeling evidenceexternal icon shows that outbreak control depends largely on the frequency of testing, the speed of reporting, and the application of interventions, and is only marginally improved by the sensitivity of the test. Additional evidenceexternal icon shows that serial antigen testing every 3 days, or twice per week, will almost always identify SARS-CoV-2 during early stages of infection, and thus significantly reduce disease transmission. Thus, if resources allow, serial antigen testing is a potentially important public health practice along with other prevention strategies.
Reporting Antigen Test Results for SARS-CoV-2 to Health Departments and Patients
A CLIA-certified laboratory or testing site must report antigen diagnostic test results to the local, state, tribal, or territory health department in accordance with Public Law 116-136, § 18115(a), the Coronavirus Aid, Relief, and Economic Security (CARES) Act. The CARES Act requires “every laboratory that performs or analyzes a test that is intended to detect SARS-CoV-2 or to diagnose a possible case of COVID-19” to report the results of each such test. Antigen test results that are reported to public health departments must be clearly distinguished from other COVID-19 tests, such as NAATs and antibody tests.
On January 8, 2021, the U.S. Department of Health and Human Services updated its published guidance on COVID-19 Pandemic Response, Laboratory Data Reportingexternal icon that specifies what additional data should be collected and electronically reported to health departments along with COVID-19 diagnostic or screening test results. Laboratory and testing professionals should collect and report complete patient demographic information and ensure that they report antigen test results using the proper LOINC code for their particular FDA-authorized tests. Facilities should refer to CDC’s LOINC In Vitro Diagnostic (LIVD) Test Code Mapping for SARS-CoV-2 Tests.
A CLIA-certified laboratory or testing site must report antigen test results to the individual or the individual’s healthcare provider according to the instructions for use of the FDA-authorized SARS-CoV-2 in vitro diagnostic device that was used. Depending on the stipulations of the FDA authorization, the laboratory or testing site may be required to report negative test results to patients as “presumptive negative.”
For long-term care facilities that are enrolled in CDC’s National Healthcare Safety Network (NHSN), the preferred method for reporting point-of-care SARS-CoV-2 testing data, including antigen test results, is through the NHSN.
Summary Table
NAATs
Antigen Tests
Intended Use
NAATs
Detect current infection
Antigen Tests
Detect current infection
Analyte Detected
NAATs
Viral Ribonucleic Acid (RNA)
Antigen Tests
Viral Antigens
Specimen Type(s)
NAATs
Nasal, Nasopharyngeal, Oropharyngeal, Sputum, Saliva
Antigen Tests
Nasal, Nasopharyngeal
Sensitivity
NAATs
Varies by test, but generally high for laboratory-based tests and moderate-to-high for POC tests
Antigen Tests
Varies depending on the course of infections, but generally moderate-to-high at times of peak viral load*
Specificity
NAATs
High
Antigen Tests
High
Test Complexity
NAATs
Varies by Test
Antigen Tests
Relatively Easy to Use+
Authorized for Use at the Point-of-Care
NAATs
Most are not, some are
Antigen Tests
Most are, some are not
Turnaround Time
NAATs
Most 1–3 days. Some could be rapid 15 minutes.
Antigen Tests
Ranges from 15 minutes–30 minutes+
Cost/Test^
NAATs
Moderate (~$75–$100/test)
Antigen Tests
Low (~$5–$50/test)
Advantages
NAATs
Most sensitive test method available
Short turnaround time for NAAT POC tests, but few available
Usually does not need to be repeated to confirm results
Antigen Tests
Short turnaround time (approximately 15 minutes)+
When performed at or near POC, allows for rapid identification of infected people, thus preventing further virus transmission in the community, workplace, etc.
Comparable performance to NAATs in symptomatic persons and/or if culturable virus present, when the person is presumed to be infectious
Disadvantages
NAATs
Longer turnaround time for lab-based tests (1–3 days)
Higher cost per test
A positive NAAT diagnostic test should not be repeated within 90 days, since people may continue to have detectable RNA after risk of transmission has passed
Antigen Tests
May need confirmatory testing
Less sensitive (more false negative results) compared to NAATs, especially among asymptomatic people
*The decreased sensitivity of antigen tests might be offset if the point-of-care antigen tests are repeated more frequently (i.e., serial testing at least weekly).
^Costs for: NAATsexternal icon, Antibody testsexternal icon
+Refers to point-of-care antigen tests only.