Division of Applied Regulatory Science Clinical Trials
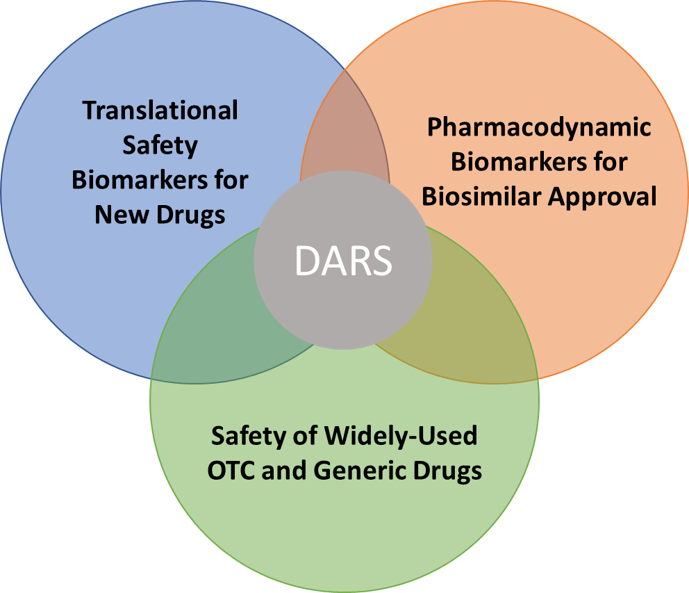
The Division of Applied Regulatory Science (DARS) conducts integrated clinical research covering clinical pharmacology, experimental medicine and postmarket analyses. DARS has greatly expanded its capability to run prospective clinical trials to address critical regulatory, drug development and public health questions.
On this page
DARS has performed or is performing clinical trials in three interconnected areas:
- Translational safety biomarkers and clinical trial methodologies to facilitate new drug development and assess the safety of marketed drugs
- Pharmacodynamic biomarkers to speed the development and availability of biosimilars
- Study design and safety evaluation focusing on widely-used over-the-counter (OTC) and generic drugs
Translational safety biomarkers and clinical trial methodologies to facilitate new drug development and assess the safety of marketed drugs
During drug development, extensive studies are performed to elucidate the safety of a product. Sometimes potential safety signals emerge in animal or other preclinical studies, but it is unclear if the safety signal translates to humans at the planned human dose levels. Thus, there is a need for biomarkers that can be used in early clinical development to monitor for potential safety signals in humans. In addition, in some cases there are biomarkers used, such as the QT interval on the electrocardiogram, which are sensitive for detecting potentially risky drugs, but are not specific. This means some drugs cause QT prolongation that is not associated with risk to patients. Thus, we need novel approaches that combine mechanistic nonclinical assays and predictive models with improved translational safety biomarkers in early development to identify which drugs are safe to proceed in clinical development. In order to advance novel translational models and biomarkers into regulatory use, DARS performs integrated nonclinical and clinical research.
DARS has completed three clinical trials and multiple additional studies assessing novel cardiac safety biomarkers
Torsade de Pointes (TdP) is a rare type of drug-induced abnormal heart rhythm. Currently, TdP risk evaluation for a new drug relies on surrogate markers of hERG potassium channel block and QT prolongation on the electrocardiogram (ECG). However, drugs can block the hERG channel or prolong QT but not cause TdP. To reduce the number of false positive signals that lead to drugs being dropped, a new Comprehensive in Vitro Proarrhythmia Assay (CiPA) paradigm was proposed. It involves assessing TdP risk using nonclinical in vitro mechanistic assays combined with in silico (computational) model predictions. When needed based on the nonclinical findings, translational safety biomarkers (focused on clinical ECG biomarker ‘J-Tpeak’ interval) can be used to confirm there are no missed or unanticipated effects. FDA has completed multiple clinical trials and studies outlined below.
Summary of Collaborative Approach to Develop Translational Safety Biomarkers
- Analysis of 34 sponsor-submitted clinical trials (>500,000 ECGs) to identify novel biomarker
- Three FDA-sponsored prospective clinical trials
- Clinical trial 1 confirming findings from retrospective analysis
- Clinical trial 2 with different drug combinations assaying the mechanism of action
- Clinical trial 3 validation study
- Further FDA-led collaborative research
- Compared additional potential biomarkers
- Reported biomarker analytical methodology and made open source code freely available
- Characterized relationship to heart rate to decrease variability and assessed sex differences
- De-identified patient-level data from all FDA-sponsored clinical trials made freely available
- Enabled multiple additional studies from industry and academia based on the FDA clinical trial data showing reproducibility with different measurement algorithms and approaches
- Discussed at public workshops/think tanks (2018 meeting), multiple summaries published and collaborative FDA-industry-academia paper on Current State of the Science (2019)
- Other investigators have published peer-reviewed articles on the use of the novel biomarkers in at least 16 nonclinical studies and 8 additional clinical studies, most in 2019-2020
Relation to ICH E14/S7B Activities: The International Council for Harmonisation (ICH) recently released a new Draft Guideline (Questions & Answers) on the Clinical and Nonclinical Evaluation of QT Prolongation and Proarrhythmic Potential. The Q&As provide specific guidance on how nonclinical data can reduce the need for clinical trials and impact regulatory decision making and labeling in certain scenarios but indicate that QT-prolonging drugs will be handled on a case-by-case basis. Specific recommendations on the combined use of nonclinical mechanistic assays with clinical ECG biomarkers for QT prolonging drugs will be discussed in a second stage of updates/Q&As to the ICH Guidelines (see ICH E14/S7B concept paper and recent public webinar).
DARS has one active clinical trial assessing pharmacokinetic and pharmacodynamic interactions between opioids and other psychotropic drugs
FDA recently added “black box” warnings to drug labels for opioids and benzodiazepines to avoid co-administration due to risk for respiratory depression. However, it is unclear whether other psychotropic drugs can have a similar effect when co-administered with opioids. DARS conducted nonclinical studies to identify other psychotropic drugs that may interact with opioids to exacerbate drug-induced respiratory depression. DARS evaluated different clinical trial methodologies and biomarkers that could be applied in phase 1-type healthy volunteer studies to assess if the potential drug interaction safety signals observed in animal models translate to effects in humans. The methodology (Read Rebreathing method) and biomarker (change in ventilation at elevated levels of carbon dioxide) are being assessed in a two-part study.
Part one will include a comparison between an opioid alone, a benzodiazepine alone, and their use together. This assessment will serve as a positive control for evaluating effects of opioids and benzodiazepines on ventilation under these study conditions. Part two will evaluate two separate sedative psychotropic drugs alone or in combination with an opioid. These sedative psychotropic drugs were selected due to their effects on ventilation in a nonclinical rat model. Findings from this study will be used to inform on the potential respiratory risk of combining select sedative psychotropic drugs with opioids, and an additional study with more sedative psychotropic drugs is planned. In addition, findings from this study may demonstrate the utility of this methodology and biomarker for evaluating effects of investigational drugs alone or in combination with other drugs (e.g., opioids, benzodiazepines) on ventilation.
Pharmacodynamic biomarkers to speed the development and availability of biosimilars
DARS has three active clinical trials on pharmacodynamic biomarkers to facilitate the availability of biosimilars
To ensure US patients realize the public health benefit of a robust, competitive market for biosimilar products, FDA is focused on improving the efficiency of biosimilar development. DARS is conducting research to inform guidance and policy on critical aspects for the use of pharmacodynamic biomarkers to demonstrate biosimilarity, which can either streamline or negate the need for comparative clinical studies. These studies will inform an evidentiary framework and methodology for identifying, characterizing and applying biomarkers to serve as primary clinical assessment for biosimilar approval. Three clinical studies are being performed on six biologic drugs (clinical trial 1 on PCSK9 biologics, clinical trial 2 on IL-5 biologics, and clinical trial 3 on interferon beta-1a biologics) to characterize biomarkers for biosimilar development. Findings from these clinical trials will increase our understanding of key study design operating characteristics and will be used to develop general policy and guidance for biosimilar product development.
Study design and safety evaluation focusing on widely-used over-the-counter and generic drugs
DARS has completed two clinical trials evaluating systemic exposure of sunscreen active ingredients
FDA has provided guidance that sunscreen active ingredients with systemic absorption in a Maximal Usage Trial (MuST) or with safety concerns should undergo expanded nonclinical toxicology assessment. Sunscreen MuST studies had not been conducted previously, so DARS developed methodology and performed two initial studies covering seven commercially-available sunscreen formulations with a combination of seven active ingredients. These studies demonstrated the feasibility of conducting a sunscreen MuST and provided critical information about the systemic absorption of sunscreen ingredients.
In the first trial, the systemic exposure of four commonly used sunscreen active ingredients was evaluated under maximal use conditions, consistent with current sunscreen labeling (i.e., apply at least every two hours). All four sunscreen active ingredients tested were absorbed. In the second trial, six active ingredients in four products were evaluated under single- and maximal-use conditions. This trial confirmed the findings from the first study and demonstrated that absorption occurred on the first day after a single full body application of sunscreen. The findings in the sunscreen absorption studies do not mean the FDA has concluded that any of the ingredients tested are unsafe for use in sunscreens, nor does the FDA seeking further information indicate that the FDA believes sunscreen active ingredients are unsafe. These trials have resulted in two JAMA publications, an editorial in ASCO, and FDA communications.
DARS has one active clinical trial evaluating the potential urinary excretion of a probable human carcinogen after ranitidine administration
Ranitidine, a medication commonly used for excessive stomach acid secretion, may contain an impurity called N-nitrosodimethylamine (NDMA) that is acceptable only at very low levels in the drug product. NDMA is classified as a probable human carcinogen based on results from laboratory tests but is also commonly found in low levels in water and multiple foods. FDA has conducted laboratory tests that simulate the potential formation of NDMA from ranitidine after it has been exposed to acid in the stomach with a normal diet. Results of these tests indicate that NDMA is not formed in typical stomach conditions or when ranitidine is exposed to small intestinal fluid. Other laboratory experiments suggest a combination of nitrites, such as those found in processed meats, and an acidic environment may increase NDMA formation; however, the levels of nitrites tested were very high. DARS is conducting a clinical study with a ranitidine product that has been tested and shown to have NDMA levels far below the acceptable daily limit. The study will determine if and how much NDMA is produced from ranitidine in the human body and whether nitrite-containing foods may increase formation of NDMA.