Nipple Aspirate Test Is No Substitute for Mammogram
A mammogram is a low-dose X-ray picture of the breast—and it’s still the best way for health care providers to screen women for breast cancer. (Breast cancer screening lets health care providers check for cancer before there are signs and symptoms of the disease.)
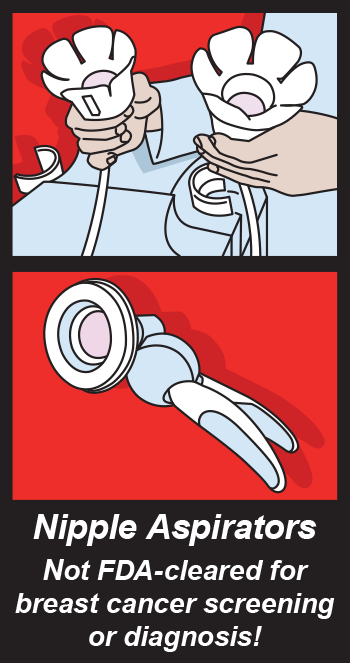
Unfortunately, in the past, other tests have been falsely described as alternatives to mammograms. One such test is the nipple aspirate, which involves drawing fluid from a woman’s breast with a special pump and testing it for abnormal cells. Companies have marketed this test as a way to screen for abnormal cells (instead of a mammogram), but the U.S. Food and Drug Administration is reminding you that this kind of test cannot be used alone to screen for or diagnose breast cancer. In fact, if women were to skip a mammogram in favor of an unproven test, it could result in serious health consequences if breast cancer goes undetected.
Furthermore, the FDA is unaware of any valid scientific data to show that a nipple aspirate test, when used on its own, is an effective screening tool for any medical condition, including the detection of breast cancer or other breast disease. And after the FDA initiated regulatory action against a company promoting such a test, the company voluntarily removed it from the market.
While the FDA believes that there are no nipple aspirate devices currently on the market, the agency urges health care providers and patients who may come in contact with the device to consider reporting it to MedWatch, the FDA’s Safety Information and Adverse Event Reporting Program.
About FDA Actions—and False Claims for Nipple Aspirate Tests
The FDA can take action when companies sell medical devices that make false medical claims. For instance, in February 2013, the FDA issued a warning letter to Atossa Genetics, Inc., a company that was selling a nipple aspirate test with false or misleading labeling touting the test as FDA-cleared. The FDA asked the firm to take prompt action to correct the violations addressed in the warning letter. In October 2013, Atossa initiated a voluntary recall to remove the ForeCYTE Breast Health Test from the market.
In addition to stating that the test can help women 18 years and older determine their risk level for breast cancer, Atossa had claimed that its test was “literally a Pap smear for breast cancer.&lrquo; (A Pap smear is a screening test for cervical cancer.) But this claim was unsubstantiated, according to FDA medical officer Michael Cummings, M.D., who reviews obstetrical and gynecological devices for the agency.
“The cervical Pap smear has a known clinical benefit supported by extensive clinical studies over many years,” Cummings says. “Its scientific ability to screen for cervical cancer is unquestioned.” The nipple aspirate test had no such evidence supporting it, he says.
A health care provider can follow up on an abnormal Pap smear with a procedure that will allow appropriately targeted biopsies. (A biopsy is a procedure that removes cells or tissue from your body to check for damage or disease.) However, an abnormal nipple aspirate report does not allow targeted biopsy to confirm the presence of diseases.
In addition, the nipple aspirate test may produce results that are falsely positive or falsely negative. (Aspirate fluid containing few cells, or no cells at all, may miss cancers and give women dangerously false reassurance.)
More Information About Mammograms
The FDA is responsible for implementing a system for certifying facilities that perform mammography—and for reviewing new mammography devices to determine whether they may be marketed—to protect the public health.
If you’re worried about how a mammogram feels, talk to your health care provider about what you can expect. A mammogram can be uncomfortable for the woman being screened because it briefly presses down on the breast to flatten out the breast tissue and increase the clarity of the X-ray image. (You also can learn more about what to expect during your mammogram, and where to find a certified mammography site, on the FDA’s website.)
Also talk with your health care provider if you have specific questions about mammography (including when or how frequently you should be screened), or if you have other questions about breast cancer screening.
The bottom line: Mammography is still the best test for breast cancer screening.