Drug Trial Snapshot: ISTURISA
HOW TO USE THIS SNAPSHOT
The information provided in Snapshots highlights who participated in the clinical trials that supported the FDA approval of this drug, and whether there were differences among sex, race and age groups. The “MORE INFO” bar shows more detailed, technical content for each section. The Snapshot is intended as one tool for consumers to use when discussing the risks and benefits of the drugs.
LIMITATIONS OF THIS SNAPSHOT:
Do not rely on Snapshots to make decisions regarding medical care. Always speak to your health provider about the risks and benefits of a drug. Refer to ISTURISA Prescribing Information for complete information.
ISTURISA (osilodrostat)
(is tur ee' sah)
Novartis
Approval date: March 6, 2020
DRUG TRIALS SNAPSHOT SUMMARY:
What is the drug for?
ISTURISA is a drug for the treatment of adults with Cushing’s disease:
- who cannot have pituitary gland surgery, or
- who have had pituitary gland surgery, but the surgery did not cure their Cushing’s disease.
Cushing’s disease is a rare disease in which the adrenal glands make too much of the cortisol hormone because of stimulation from a pituitary tumor.
How is this drug used?
ISTURISA is a tablet that is taken two times a day (approximately every 12 hours).
What are the benefits of this drug?
In the clinical trial, about half of the patients who received ISTURISA had cortisol levels within normal limits at the end of the 24-week treatment period. Of these patients, 86% of patients receiving ISTURISA maintained cortisol levels within normal limits compared to 30% of patients taking the placebo at the end of the following 8-week period.
What are the benefits of this drug (results of trials used to assess efficacy)?
The tables below present efficacy assessments of ISTURISA. The primary endpoint was based on the percentage of patients with normal mean urine free cortisol (mUFC) at the end of Period 3. The key secondary endpoint was a complete responder rate after the first 24 weeks of treatment with ISTURISA.
Table 1. Percentage of Cushing’s Disease Patients with Normal mUFC at End of Period 3 (8-week randomized withdrawal period)
|
Primary Endpoint
|
ISTURISA (N = 36) n (%) |
Placebo (N = 34) n (%) |
Complete Responder Rate Difference (Differences in Percentages) |
|---|---|---|---|
|
Complete responder rate at the end of (95% CI) |
31 (86)
(71, 95) |
10 (29)
(15, 47) |
ISTURISA vs placebo
57 (38, 76) 2-sided p-value < 0.001 |
Abbreviation: CI, Confidence Interval.
ISTURISA Prescribing Information
Table 2. Percent Patients Achieving Normal Cortisol Levels After 24 Weeks of Treatment
|
Trial 1 |
Percent (n/N) |
95% Confidence Interval |
|---|---|---|
|
53% (75/137) |
(44%, 61%) |
FDA Statistical Review for Drug Trials Snapshot
Were there any differences in how well the drug worked in clinical trials among sex, race and age?
- Sex: ISTURISA worked similarly in men and women.
- Race: ISTURISA worked similarly in White and Asian patients. The number of patients of other races was limited; therefore, differences among other races could not be determined.
- Age: The number of patients 65 years of age or older was limited; therefore, differences between patients above and below 65 years of age could not be determined.
Were there any differences in how well the drug worked in clinical trials among sex, race, and age groups?
Analyses of efficacy assessments by subgroups are presented below.
Table 3. Percent Patients Achieving Normal Cortisol Levels After 24 Weeks of Treatment by Subgroups
|
Demographic Parameter |
Percent % (n/N) |
|
|---|---|---|
|
|
ISTURISA % (n/N) |
95% Confidence Interval |
|
Sex |
||
|
Men |
58% (18/31) |
(39%, 76%) |
|
Women |
51% (54/106) |
(41%, 61%) |
|
Race |
||
|
White |
58% (52/89) |
(48%, 68%) |
|
Asian |
36% (14/39) |
(21%, 53%) |
|
Black or African American |
75% (3/4) |
(19%, 99%) |
|
Age Group (Years) |
||
|
< 65 |
53% (69/130) |
(44%, 62%) |
|
≥ 65 |
43% (3/7) |
(10%, 82%) |
Table 4. Effects of ISTURISA on Percent of Patients with Sustained Response for at Least Two Months
|
Demographic Parameter |
Complete Resp. % (n/N) |
Treatment Differencea |
|
|---|---|---|---|
|
Placebo |
ISTURISA |
(95% CI) |
|
|
Sex |
|||
|
Men |
31% (4/13) |
50% (3/6) |
19% (-28%, 67%) |
|
Women |
29% (6/21) |
93% (28/30) |
65% (43%, 86%) |
|
Race |
|||
|
White |
36% (8/22) |
85% (23/27) |
49% (25%, 73%) |
|
Asian |
29% (2/7) |
86% (6/7) |
57% (15%, 99%) |
|
Age Group (years) |
|||
|
< 65 |
30% (10/33) |
85% (29/34) |
55% (35%, 75%) |
a Patients who discontinued treatment or were missing data at week of evaluation were considered to be without a sustained response.
FDA Statistical Review for Drug Trials Snapshot
What are the possible side effects?
ISTURISA may cause serious side effects including low cortisol levels in the blood, heart rhythm problems due to prolongation of heart electrical activity (QT prolongation) and symptoms associated with an increase in other adrenal hormone levels.
The most common side effects were hypoactive adrenal glands (adrenal insufficiency), fatigue, nausea, headache and leg and ankle swelling.
What are the possible side effects (results of trials used to assess safety)?
Adverse reactions that occurred in the trial are presented below.
Table 5. Adverse Reactions with Frequency of > 10% in 48-week Clinical Trial in Cushing’s Disease Patients
|
Adverse Reaction Type |
(N = 137) % |
|---|---|
|
Adrenal insufficiencya |
43.1 |
|
Fatigueb |
38.7 |
|
Nausea |
37.2 |
|
Headachec |
30.7 |
|
Edemad |
21.2 |
|
Nasopharyngitis |
19.7 |
|
Vomiting |
19 |
|
Arthralgia |
17.5 |
|
Back pain |
15.3 |
|
Rashe |
15.3 |
|
Diarrhea |
14.6 |
|
Blood corticotrophin increased |
13.9 |
|
Dizzinessf |
13.9 |
|
Abdominal paing |
13.1 |
|
Hypokalaemiah |
12.4 |
|
Myalgia |
12.4 |
|
Decreased appetite |
11.7 |
|
Hormone level abnormal |
11.7 |
|
Hypotensioni |
11.7 |
|
Urinary tract infection |
11.7 |
|
Blood testosterone increased |
10.9 |
|
Anemia |
10.2 |
|
Cough |
10.2 |
|
Hypertension |
10.2 |
|
Influenza |
10.2 |
a Adrenal insufficiency includes glucocorticoid deficiency, adrenocortical insufficiency acute, steroid withdrawal syndrome, cortisol free urine decreased, cortisol decreased. One-third of the subjects with this event had low cortisol levels indicative of Adrenal Insufficiency. The majority of subjects had normal cortisol levels suggesting a cortisol withdrawal syndrome.
b Fatigue includes lethargy, asthenia.
c Headache includes head discomfort.
d Edema includes edema peripheral, generalized edema, localized edema.
e Rash includes rash erythematous, rash generalized, rash maculopapular, rash papular.
f Dizziness includes dizziness postural.
g Abdominal pain includes abdominal pain upper, abdominal discomfort
h Hypokalaemia includes blood potassium decreased.
i Hypotension includes orthostatic hypotension, blood pressure decreased, blood pressure diastolic decreased, blood pressure systolic decreased.
ISTURISA Prescribing Information
Were there any differences in side effects among sex, race and age?
- Sex: The occurrence of side effects was similar in men and women.
- Race: The occurrence of overall side effects was similar in White and Asian patients; the occurrence of endocrine side effects was higher in Asians. The number of patients of other races was limited; therefore, differences in side effects among other races could not be determined.
- Age: The number of patients 65 years of age or older was limited; therefore, differences in side effects between patients above and below 65 years of age could not be determined.
Were there any differences in side effects of the clinical trials among sex, race, and age groups?
The occurrence of treatment emergent adverse events was 100% in all demographic subgroups. The table below summarizes adverse reactions in endocrine disorders system organ class (SOC) by subgroups.
Table 6. Subgroup Analyses of Adverse Reactions in Endocrine Disorders SOC
|
Demographic Parameters |
ISTURISA n/N (%) |
|---|---|
|
Sex |
|
|
Men |
14 (45.2) |
|
Women |
55 (51.9) |
|
Race |
|
|
White |
38 (42.7) |
|
Black or African American |
2 (50) |
|
Asian |
27 (69.2) |
|
Other |
2 (40) |
|
Age Group |
|
|
>65 years |
65 (50) |
|
≥ 65 years |
4 (57.1) |
Clinical Trial Data
WHO WAS IN THE CLINICAL TRIALS?
Who participated in the clinical trials?
The FDA approved ISTURISA based on the evidence from one clinical trial (NCT02180217) of 137 patients with Cushing’s disease.
The trial was conducted at 66 sites across 19 countries (United States, Argentina, Austria, Bulgaria, Canada, China, Columbia, Germany, Spain, France, Great Britain, India, Italy, Japan, Korea, Netherlands, Russia, Thailand, and Turkey).
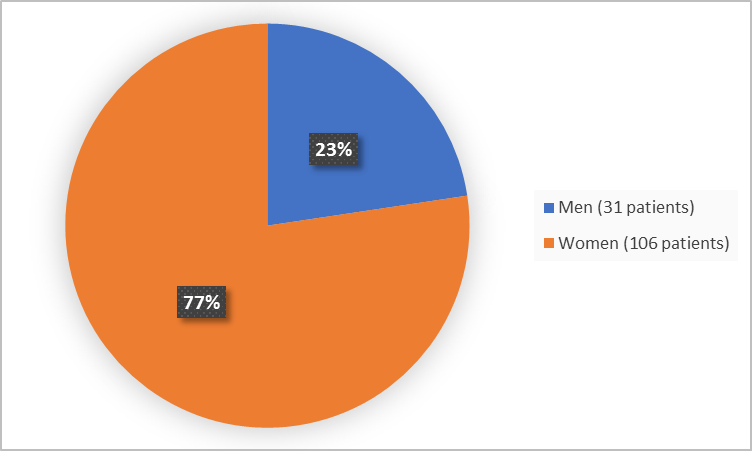
Figure below summarizes how many men and women were in the clinical trial.
Figure 1. Baseline Demographics by Sex (safety population)
FDA Clinical Review
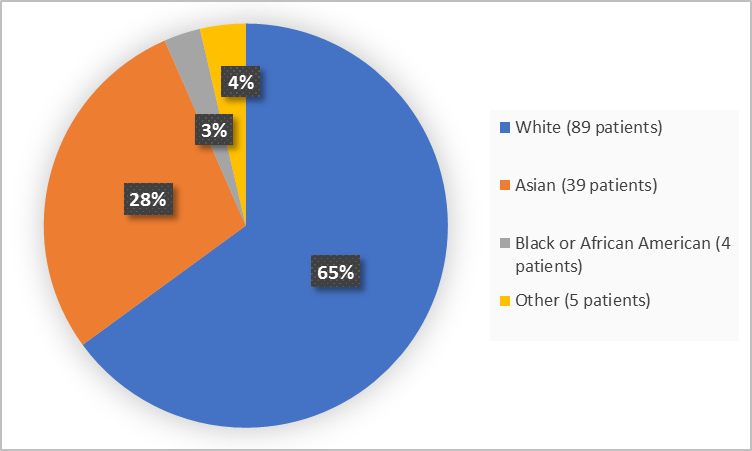
Figure below summarizes the percentage of patients by race in the clinical trial.
Figure 2. Baseline Demographics by Race (safety population)
FDA Clinical Review
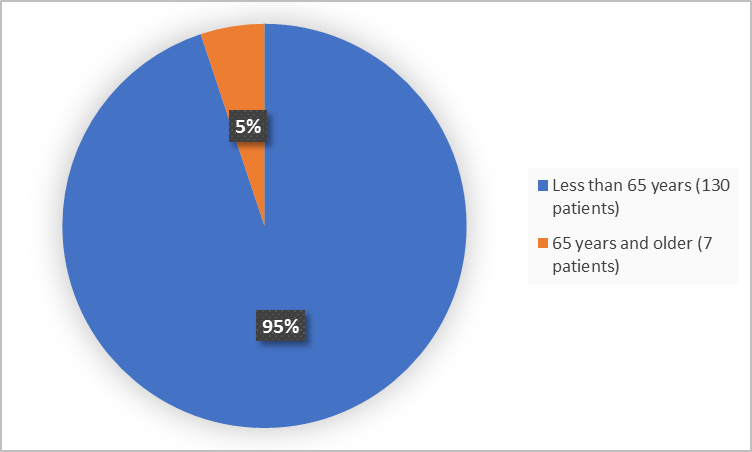
Figure below summarizes the percentage of patients by age in the clinical trial.
Figure 3. Baseline Demographics by Age (safety population)
FDA Clinical Review
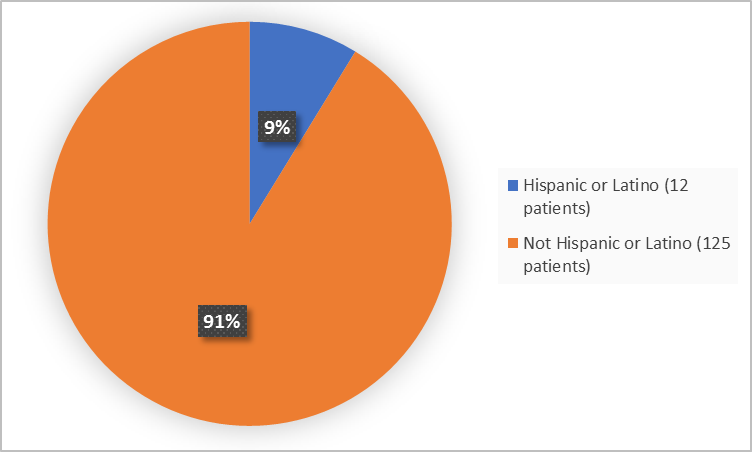
Figure below summarizes the percentage of patients by ethnicity in the clinical trial.
Figure 4. Baseline Demographics by Ethnicity (safety population)
FDA Clinical Review
Who participated in the trials?
The table presents demographics of the trial safety population.
Table 7. Trial Demographics (safety population)
|
|
Total (N=137) n (%) |
|---|---|
|
Sex |
|
|
Men |
31 (22.6) |
|
Women |
106 (77.4) |
|
Race |
|
|
White |
89 (65) |
|
Black or African American |
4 (2.9) |
|
Asian |
39 (28.5) |
|
Other |
5 (3.6) |
|
Age (years) |
|
|
Median |
40 |
|
Min, Max |
10-70 |
|
Age Group |
|
|
< 65 years |
130 (94.9) |
|
≥ 65 years |
7 (5.1) |
|
Ethnicity |
|
|
Hispanic or Latino |
12 (8.8) |
|
Not Hispanic or Latino |
125 (91.2) |
|
Region |
|
|
USA |
25 (18.2) |
|
All Other* |
112 (81.8) |
*Argentina, Austria, Bulgaria, Canada, China, Columbia, Germany, Spain, France, Great Brittan, India, Italy, Japan, Korea, Netherlands, Russia, Thailand, and Turkey
FDA Clinical Review
How were the trials designed?
There was one trial of 48 weeks duration that assessed the benefits and side effects of ISTURISA. The trial enrolled patients with Cushing’s disease for whom pituitary gland surgery was not an option or did not work.
The trial was divided in 4 periods. Patients received ISTURISA two times a day in all 4 periods. After the first two periods (24 weeks), the benefit of ISTURISA was assessed by the percentage of patients who had 24-hour urinary free cortisol levels within normal limits.
In the third period (which lasted 8 weeks), half of the patients who had normal urinary free cortisol levels after 24 weeks of treatment continued taking ISTURISA and the other half was switched to placebo. Neither the patients nor the healthcare providers know which treatment was given during this period. The benefit of ISTURISA was assessed on the percentage of patients who had normal cortisol levels at the end of this period versus the patients who received placebo.
How were the trials designed?
The safety and efficacy of ISTURISA were evaluated in a multicenter, 48-week trial that enrolled Cushing’s disease patients with persistent or recurrent disease despite pituitary surgery or de novo patients for whom surgery was not indicated or who had refused surgery. The trial consisted of four periods as follows:
- Period 1: 12-week, open-label, dose titration period
- Period 2: 12-week, open-label, maintenance treatment period
- Period 3: 8-week, double-blind, placebo-controlled, randomized withdrawal treatment period which provided the data for the primary efficacy endpoint
- Period 4: open-label treatment period of 14 to 24 weeks duration
The primary efficacy endpoint was the percentage of complete responders at the end of the 8- week randomized withdrawal period (Period 3) between patients randomized to continue ISTURISA versus the patients switched to placebo. A complete responder for the primary endpoint was defined as a patient who had mUFC ≤ ULN based on central laboratory results at the end of Period 3 (Week 34), and who neither discontinued randomized treatment or the study nor had any dose increase above their Week 26 dose. The key secondary endpoint was a complete responder rate after the first 24 weeks of treatment with ISTURISA.
GLOSSARY
CLINICAL TRIAL: Voluntary research studies conducted in people and designed to answer specific questions about the safety or effectiveness of drugs, vaccines, other therapies, or new ways of using existing treatments.
COMPARATOR: A previously available treatment or placebo used in clinical trials that is compared to the actual drug being tested.
EFFICACY: How well the drug achieves the desired response when it is taken as described in a controlled clinical setting, such as during a clinical trial.
PLACEBO: An inactive substance or “sugar pill” that looks the same as, and is given the same way as, an active drug or treatment being tested. The effects of the active drug or treatment are compared to the effects of the placebo.
SUBGROUP: A subset of the population studied in a clinical trial. Demographic subsets include sex, race, and age groups.
LINK TO PRESCRIBING INFORMATION