induced Pluripotent Stem cells
Studying Color Vision in a Dish
Posted on by Dr. Francis Collins

Credit: Eldred et al., Science
Researchers can now grow miniature versions of the human retina—the light-sensitive tissue at the back of the eye—right in a lab dish. While most “retina-in-a-dish” research is focused on finding cures for potentially blinding diseases, these organoids are also providing new insights into color vision.
Our ability to view the world in all of its rich and varied colors starts with the retina’s light-absorbing cone cells. In this image of a retinal organoid, you see cone cells (blue and green). Those labelled with blue produce a visual pigment that allows us to see the color blue, while those labelled green make visual pigments that let us see green or red. The cells that are labeled with red show the highly sensitive rod cells, which aren’t involved in color vision, but are very important for detecting motion and seeing at night.
Snapshots of Life: Growing Mini-Brains in a Dish
Posted on by Dr. Francis Collins
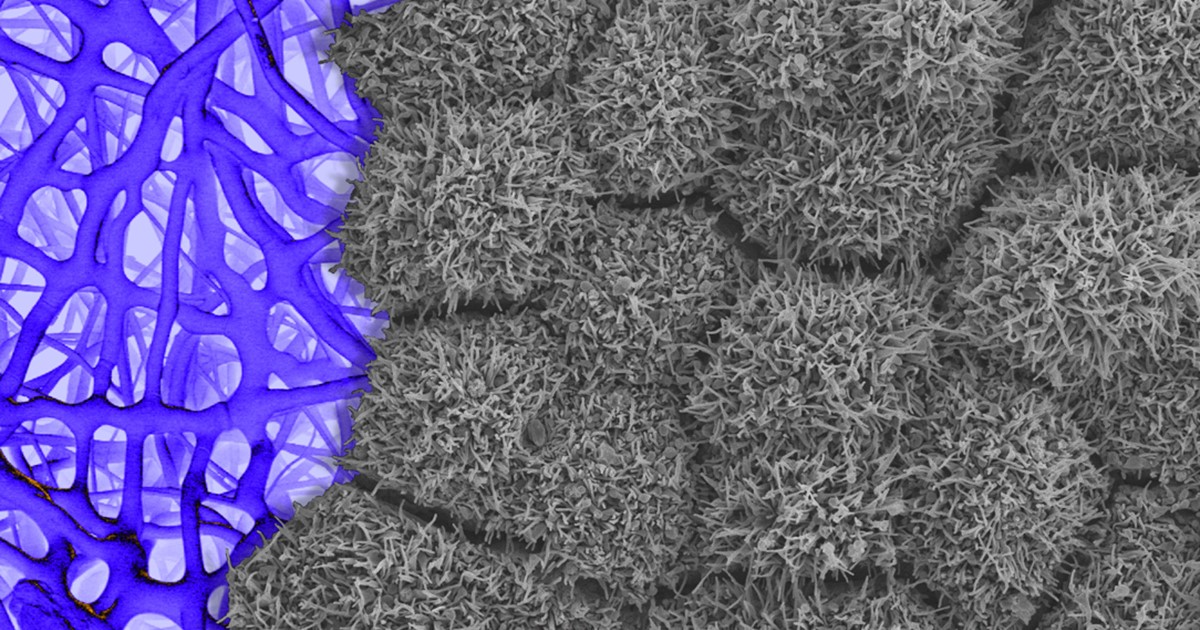
Something pretty incredible happens—both visually and scientifically—when researchers spread neural stem cells onto a gel-like matrix in a lab dish and wait to see what happens. Gradually, the cells differentiate and self-assemble to form cohesive organoids that resemble miniature brains!
In this image of a mini-brain organoid, the center consists of a clump of neuronal bodies (magenta), surrounded by an intricate network of branching extensions (green) through which these cells relay information. Scattered throughout the mini-brain are star-shaped astrocytes (red) that serve as support cells.
Creative Minds: Mapping the Biocircuitry of Schizophrenia and Bipolar Disorder
Posted on by Dr. Francis Collins
As a graduate student in the 1980s, Bruce Yankner wondered what if cancer-causing genes switched on in non-dividing neurons of the brain. Rather than form a tumor, would those genes cause neurons to degenerate? To explore such what-ifs, Yankner spent his days tinkering with neural cells, using viruses to insert various mutant genes and study their effects. In a stroke of luck, one of Yankner’s insertions encoded a precursor to a protein called amyloid. Those experiments and later ones from Yankner’s own lab showed definitively that high concentrations of amyloid, as found in the brains of people with Alzheimer’s disease, are toxic to neural cells [1].
The discovery set Yankner on a career path to study normal changes in the aging human brain and their connection to neurodegenerative diseases. At Harvard Medical School, Boston, Yankner and his colleague George Church are now recipients of an NIH Director’s 2016 Transformative Research Award to apply what they’ve learned about the aging brain to study changes in the brains of younger people with schizophrenia and bipolar disorder, two poorly understood psychiatric disorders.
Creative Minds: A Transcriptional “Periodic Table” of Human Neurons
Posted on by Dr. Francis Collins

Caption: Mouse fibroblasts converted into induced neuronal cells, showing neuronal appendages (red), nuclei (blue) and the neural protein tau (yellow).
Credit: Kristin Baldwin, Scripps Research Institute, La Jolla, CA
Writers have The Elements of Style, chemists have the periodic table, and biomedical researchers could soon have a comprehensive reference on how to make neurons in a dish. Kristin Baldwin of the Scripps Research Institute, La Jolla, CA, has received a 2016 NIH Director’s Pioneer Award to begin drafting an online resource that will provide other researchers the information they need to reprogram mature human skin cells reproducibly into a variety of neurons that closely resemble those found in the brain and nervous system.
These lab-grown neurons could be used to improve our understanding of basic human biology and to develop better models for studying Alzheimer’s disease, autism, and a wide range of other neurological conditions. Such questions have been extremely difficult to explore in mice and other animal models because they have shorter lifespans and different brain structures than humans.
Regenerative Medicine: Making Blood Stem Cells in the Lab
Posted on by Dr. Francis Collins

Caption: Arrow in first panel points to an endothelial cell induced to become hematopoietic stem cell (HSC). Second and third panels show the expansion of HSCs over time.
Credit: Raphael Lis, Weill Cornell Medicine, New York, NY
Bone marrow transplants offer a way to cure leukemia, sickle cell disease, and a variety of other life-threatening blood disorders.There are two major problems, however: One is many patients don’t have a well-matched donor to provide the marrow needed to reconstitute their blood with healthy cells. Another is even with a well-matched donor, rejection or graft versus host disease can occur, and lifelong immunosuppression may be needed.
A much more powerful option would be to develop a means for every patient to serve as their own bone marrow donor. To address this challenge, researchers have been trying to develop reliable, lab-based methods for making the vital, blood-producing component of bone marrow: hematopoietic stem cells (HSCs).
Two new studies by NIH-funded research teams bring us closer to achieving this feat. In the first study, researchers developed a biochemical “recipe” to produce HSC-like cells from human induced pluripotent stem cells (iPSCs), which were derived from mature skin cells. In the second, researchers employed another approach to convert mature mouse endothelial cells, which line the inside of blood vessels, directly into self-renewing HSCs. When these HSCs were transplanted into mice, they fully reconstituted the animals’ blood systems with healthy red and white blood cells.
LabTV: Curious About Parkinson’s Disease
Posted on by Dr. Francis Collins
When the young scientist featured in this LabTV video first learned about induced pluripotent stem (iPS) cells a few years ago as an undergrad, he thought it would be cool if he could someday work with this innovative technology. Today, as a graduate student, Kinsley Belle is part of a research team that’s using iPS cells on a routine basis to gain a deeper understanding of Parkinson’s disease.
Derived from genetically reprogrammed skin cells or white blood cells, iPS cells have the potential to develop into many different types of cells, providing scientists with a powerful tool to model a wide variety of diseases in laboratory dishes. At the University of Miami’s John P. Hussman Institute for Human Genomics, Belle and his colleagues are taking advantage of an iPS model of Parkinson’s disease to explore its molecular roots. Their goal? To use that information to develop better treatments or maybe even a cure for the neurodegenerative disorder that affects at least a half-million Americans.
Bioengineering: Big Potential in Tiny 3D Heart Chambers
Posted on by Dr. Francis Collins

Caption: Heart microchamber generated from human iPS cells; cardiomyocytes (red), myofibroblasts (green), cell nuclei (blue)
Credit: Zhen Ma, University of California, Berkeley
The adult human heart is about the size of a large fist, divided into four chambers that beat in precise harmony about 100,000 times a day to circulate blood throughout the body. That’s a very dynamic system, and also a very challenging one to study in real-time in the lab. Understanding how the heart forms within developing human embryos is another formidable challenge. So, you can see why researchers are excited by the creation of tiny, 3D heart chambers with the ability to exist (see image above) and even beat (see video below) in a lab dish, or as scientists say “in vitro.”
To achieve this feat, an NIH-funded team from University of California, Berkeley, and Gladstone Institute of Cardiovascular Disease, San Francisco turned to human induced pluripotent stem (iPS) cell technology. The resulting heart chambers may be miniscule—measuring no more than a couple of hair-widths across—but they hold huge potential for everything from improving understanding of cardiac development to speeding drug toxicity screening.
Next Page