microcephaly
Study Shows Genes Unique to Humans Tied to Bigger Brains
Posted on by Dr. Francis Collins

Caption: Cortical organoid, showing radial glial stem cells (green) and cortical neurons (red).
Credit: Sofie Salama, University of California, Santa Cruz
In seeking the biological answer to the question of what it means to be human, the brain’s cerebral cortex is a good place to start. This densely folded, outer layer of grey matter, which is vastly larger in Homo sapiens than in other primates, plays an essential role in human consciousness, language, and reasoning.
Now, an NIH-funded team has pinpointed a key set of genes—found only in humans—that may help explain why our species possesses such a large cerebral cortex. Experimental evidence shows these genes prolong the development of stem cells that generate neurons in the cerebral cortex, which in turn enables the human brain to produce more mature cortical neurons and, thus, build a bigger cerebral cortex than our fellow primates.
That sounds like a great advantage for humans! But there’s a downside. Researchers found the same genomic changes that facilitated the expansion of the human cortex may also render our species more susceptible to certain rare neurodevelopmental disorders.
Tracing Spread of Zika Virus in the Americas
Posted on by Dr. Francis Collins
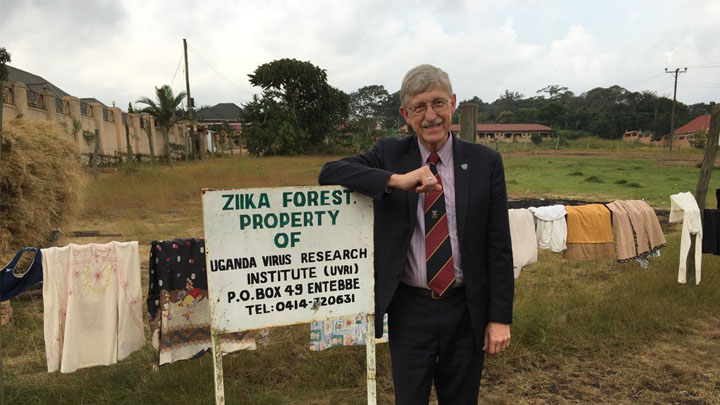
Caption: Here I am visiting the Ziika Forest area of Uganda, where the Zika virus was first identified in 1947.
Credit: National Institutes of Health
A couple of summers ago, the threat of mosquito-borne Zika virus disease in tropical areas of the Americas caused major concern, and altered the travel plans of many. The concern was driven by reports of Zika-infected women giving birth to babies with small heads and incompletely developed brains (microcephaly), as well as other serious birth defects. So, with another summer vacation season now upon us, you might wonder what’s become of Zika.
While pregnant women and couples planning on having kids should still take extra precautions [1] when travelling outside the country, the near-term risk of disease outbreaks has largely subsided because so many folks living in affected areas have already been exposed to the virus and developed protective immunity. But the Zika virus—first identified in the Ziika Forest in Uganda in 1947—has by no means been eliminated, making it crucial to learn more about how it spreads to avert future outbreaks. It’s very likely we have not heard the last of Zika in the Western hemisphere.
Recently, an international research team, partly funded by NIH, used genomic tools to trace the spread of the Zika virus. Genomic analysis can be used to build a “family tree” of viral isolates, and such analysis suggests that the first Zika cases in Central America were reported about a year after the virus had actually arrived and begun to spread.
The Zika virus, having circulated for decades in Africa and Asia before sparking a major outbreak in French Polynesia in 2013, slipped undetected across the Pacific Ocean into Brazil early in 2014, as established in previous studies. The new work reveals that by that summer, the bug had already hopped unnoticed to Honduras, spreading rapidly to other Central American nations and Mexico—likely by late 2014 and into 2015 [2].
Treating Zika Infection: Repurposed Drugs Show Promise
Posted on by Dr. Francis Collins

Credit: National Center for Advancing Translational Sciences, NIH
In response to the health threat posed by the recent outbreak of Zika virus in Latin America and its recent spread to Puerto Rico and Florida, researchers have been working at a furious pace to learn more about the mosquito-borne virus. Considerable progress has been made in understanding how Zika might cause babies to be born with unusually small heads and other abnormalities and in developing vaccines that may guard against Zika infection.
Still, there remains an urgent need to find drugs that can be used to treat people already infected with the Zika virus. A team that includes scientists at NIH’s National Center for Advancing Translational Sciences (NCATS) now has some encouraging news on this front. By testing 6,000 FDA-approved drugs and experimental chemical compounds on Zika-infected human cells in the lab, they’ve shown that some existing drugs might be repurposed to fight Zika infection and prevent the virus from harming the developing brain [1]. While additional research is needed, the new findings suggest it may be possible to speed development and approval of new treatments for Zika infection.
Zika Vaccine: Two Candidates Show Promise in Mice
Posted on by Dr. Francis Collins

Caption: Zika virus (red), isolated from a microcephaly case in Brazil. The virus is associated with cellular membranes in the center.
Credit: NIAID
Last February, the World Health Organization declared a public health emergency over concerns about very serious birth defects in Brazil and their possible link to Zika virus. But even before then, concerns about the unprecedented spread of Zika virus in Brazil and elsewhere in Latin America had prompted NIH-funded scientists to step up their efforts to combat this emerging infectious disease threat. Over the last year, research aimed at understanding the mosquito-borne virus has progressed rapidly, and we now appear to be getting closer to a Zika vaccine.
In a recent study in the journal Nature, researchers found that a single dose of either of two experimental vaccines completely protected mice against a major viral strain responsible for the Zika outbreak in Brazil [1]. Caution is certainly warranted when extrapolating these (or any other) findings from mice to people. But, taking into account the fact that researchers have already developed safe and effective human vaccines for several related viruses, the new work represents a very encouraging milestone on the road toward a much-needed Zika vaccine for humans.
Zika and Birth Defects: The Evidence Mounts
Posted on by Dr. Francis Collins

Caption: Human neural progenitor cells (gray) infected with Zika virus (green) increased the enzyme caspase-3 (red), suggesting increased cell death.
Credit: Sarah C. Ogden, Florida State University, Tallahassee
Recently, public health officials have raised major concerns over the disturbing spread of the mosquito-borne Zika virus among people living in and traveling to many parts of Central and South America [1]. While the symptoms of Zika infection are typically mild, grave concerns have arisen about its potential impact during pregnancy. The concerns stem from the unusual number of births of children with microcephaly, a very serious condition characterized by a small head and damaged brain, coinciding with the spread of Zika virus. Now, two new studies strengthen the connection between Zika and an array of birth defects, including, but not limited to, microcephaly.
In the first study, NIH-funded laboratory researchers show that Zika virus can infect and kill human neural progenitor cells [2]. Those progenitor cells give rise to the cerebral cortex, a portion of the brain often affected in children with microcephaly. The second study, involving a small cohort of women diagnosed with Zika virus during their pregnancies in Rio de Janeiro, Brazil, suggests that the attack rate is disturbingly high, and microcephaly is just one of many risks to the developing fetus. [3]
