
Posted April 12, 2024. Past health advisories and alerts are archived for historical purposes and are not maintained or updated.
Summary
Washington State is not seeing an increase in meningococcal disease. The preliminary case count for 2023 is four confirmed cases, and three confirmed cases have been reported to-date in 2024. We are sharing this Health Advisory for your situational awareness.
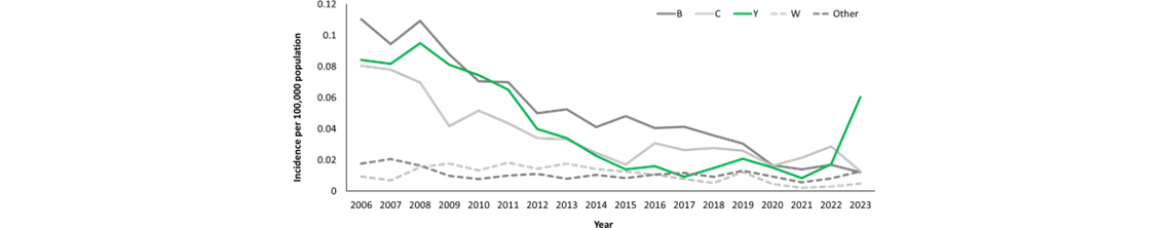
The Centers for Disease Control and Prevention (CDC) is issuing this Health Alert Network (HAN) Health Advisory to alert healthcare providers to an increase in invasive meningococcal disease, mainly attributable to Neisseria meningitidis serogroup Y (Figure). In 2023, 422 cases were reported in the United States, the highest annual number of cases reported since 2014. As of March 25, 2024, 143 cases have been reported to CDC for the current calendar year, an increase of 62 cases over the 81 reported as of this date in 2023. A specific meningococcal strain, sequence type (ST) 1466, is responsible for most (101 of 148, 68%) serogroup Y cases with available sequence type data that were reported across the United States in 2023.
Cases caused by this strain are disproportionately occurring in people ages 30–60 years (65%), Black or African American people (63%), and people with HIV (15%). In addition, most cases of invasive meningococcal disease caused by ST-1466 in 2023 had a clinical presentation other than meningitis: 64% presented with bacteremia, and at least 4% presented with septic arthritis. Of 94 patients with known outcomes, 17 (18%) died; this case-fatality rate is higher than the historical case-fatality rate of 11% reported for serogroup Y cases in 2017–2021.
Healthcare providers should:
Background
Meningococcal disease, caused by the bacterium Neisseria meningitidis, is a rare but severe illness with a case-fatality rate of 10–15% even with appropriate antibiotic treatment. Meningococcal disease most often presents as meningitis, with symptoms that may include fever, headache, stiff neck, nausea, vomiting, photophobia, or altered mental status; or as meningococcal bloodstream infection, with symptoms that may include fever and chills, fatigue, vomiting, cold hands and feet, severe aches and pains, rapid breathing, diarrhea, or, in later stages, a dark purple rash. While initial symptoms of meningococcal disease can at first be non-specific, they worsen rapidly, and the disease can become life-threatening within hours. Immediate antibiotic treatment for meningococcal disease is critical. Survivors may experience long-term effects such as deafness or amputations of the extremities.
Of the six N. meningitidis serogroups — A, B, C, W, X, and Y — responsible for most meningococcal disease worldwide, the four serogroups B, C, W, and Y circulate in the United States. Vaccines against serogroups A, C, W, Y (MenACWY) and serogroup B (MenB) are available in the United States. MenACWY vaccines are routinely recommended for adolescents and for people with other risk factors or underlying medical conditions, including HIV.
The serogroup Y ST-1466 strain has contributed to previously reported increases in meningococcal disease in people with HIV. Based on updated surveillance data, 24 ST-1466 cases have now been reported in people with HIV in 2022–2023; only four were previously vaccinated with MenACWY and none were up to date on recommended doses. To date, no other ST-1466 cases have been identified in people who previously received MenACWY vaccine.
Serogroup Y ST-1466 isolates tested to date have been susceptible to all first-line antibiotics recommended for treatment and prophylaxis. This strain is distinct from ciprofloxacin-resistant serogroup Y strains that are also circulating in the United States and that are disproportionately affecting Hispanic individuals.
Figure: Trends in meningococcal disease incidence per 100,000 population, by serogroup—United States, 2006–2023. Incidence of Neisseria meningitidis serogroup Y is shown in green. Source: National Notifiable Diseases Surveillance System, with additional serogroup data from Active Bacterial Core surveillance (ABCs) and state health departments. 2022 and 2023 data are preliminary.
Recommendations for Healthcare Providers
Recommendations for the Public
For More Information
Healthcare providers
Everyone
Contact SRHD at 509-324-1442 or CDEpi@srhd.org with any additional questions.