Posted Nov. 14, 2018. Past health advisories and alerts are archived for historical purposes and are not maintained or updated.
At least 25 high school students and staff members at Upper Columbia Academy (UCA) in Spangle, WA have compatible illness with B. pertussis, including two lab-confirmed cases. The onset of the outbreak was mid-September; however, the first lab confirmed case was identified late last week. UCA is a private Seventh-day Adventist boarding school for approximately 200 high school students from the Northwest and all over the country. A small elementary school for local students and a church attended by students, staff, and local families are also present on the UCA campus.
Given the large numbers of ill students and staff, SRHD is considering the following groups to be exposed:
*Examples of close contact include direct face-to-face contact; an obvious exposure that involves direct contact with respiratory, oral, or nasal secretions from a case-patient (a cough/sneeze in the face, kissing, sharing eating utensils, etc.), and close proximity for a prolonged period of time (risk of exposure increases with longer duration and closer proximity of contact). Close contact does NOT include activities such as walking by a person or briefly sitting across a waiting room or office from someone.
CDC and SRHD support targeting post-exposure prophylaxis (PEP) antibiotic use for people at high risk of developing severe pertussis, as well as people who will have close contact with others at high risk of developing severe disease. Due to the close-knit, family community of UCA, SRHD supports the use of PEP in exposed students and families at the campus within 21 days of exposure as follows:
No illnesses have been confirmed in the elementary school at this time. However, there is some interaction between elementary and high school students at UCA and exposure assessments should be done individually.
If after assessing exposure it is not clear whether an exposure occurred, it is appropriate to encourage the exposed person to watch for signs and symptoms of pertussis for 21 days following their last exposure to a symptomatic person. These exposed persons should be instructed to seek healthcare immediately at the first sign of compatible illness
Pertussis, more commonly known as whooping cough, is a contagious, respiratory disease caused by the bacterium Bordetella pertussis. The illness is typically characterized by a prolonged paroxysmal cough that is often accompanied by an inspiratory whoop. Disease presentation can vary with age and history of previous exposure or vaccination. Young infants may present to a clinic or hospital with apnea and no other disease symptoms. Adolescents and adults with some immunity may exhibit only mild symptoms or have the typical prolonged paroxysmal cough. In all persons, cough can continue for months. Infants are at greatest risk for pertussis-related complications and mortality. The Centers for Disease Control & Prevention (CDC) maintains a thorough overview of the clinical features of each stage of illness.
Early diagnosis and treatment of pertussis might limit its spread to other susceptible people. When pertussis is strongly suspected, attempts to identify and provide prophylaxis to household and other close contacts at high risk should proceed without waiting for laboratory confirmation.
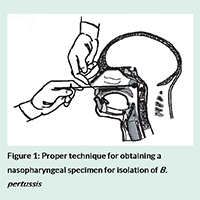
Determining who has pertussis and who does not can be difficult, particularly during the catarrhal phase when symptoms can be indistinguishable from those of minor respiratory tract infections (coryza, low-grade fever, mild cough). Whenever possible, a nasopharyngeal swab should be obtained from all persons with suspected pertussis for PCR testing. A properly obtained nasopharyngeal swab or aspirate is essential for diagnosis. CDC has produced training videos on proper specimen collection.
Antimicrobial treatment does not generally lessen the severity of disease unless it is begun in the catarrhal phase, prior to paroxysmal coughing. However, early treatment reduces transmission and is essential for disease control. Persons with pertussis are infectious from the beginning of the catarrhal stage through the third week after the onset of paroxysms or until five days after the start of effective antimicrobial treatment.
The recommended antimicrobial agents and doses are the same for both treatment and chemoprophylaxis. Three macrolides are recommended by CDC for treatment of pertussis. Azithromycin is most popular because it is given in a short, simple regimen of one dose each day for five days. Full treatment guidelines are available from the CDC.
Vaccination is the most effective way to prevent pertussis. Babies and children should get five doses of DTaP for maximum protection. A booster dose of Tdap is given to preteens at 11 or 12 years old. Teens or adults who didn’t get Tdap as a preteen should get one dose. Pregnant women should also receive a dose of Tdap during each pregnancy in the third trimester.
Pertussis vaccines are effective, but not perfect. They typically offer good levels of protection within the first two years after getting the vaccine, but then protection wanes over time. In general, DTaP vaccines are 80% to 90% effective. Among children who get all five doses of DTaP on schedule, effectiveness is very high within the year following the 5th dose – at least nine out of ten kids are fully protected. There is a modest decrease in effectiveness in each following year. About seven out of ten kids are fully protected five years after getting their last dose of DTaP and the other three out of ten kids are partially protected – protecting against serious disease.
CDC’s current estimate is that in the first year after getting vaccinated with Tdap, it protects about seven out of ten people who receive it. There is a decrease in effectiveness in each following year. About three or four out of ten people are fully protected four years after getting Tdap.